HISTORY and BACKGROUND
Non-Digital Occlusion
Dentistry has struggled for many years to reach a consensus and understanding of the complex, and often philosophically muddled topic of Occlusion. Dental schools and many occlusal continuums still persist in teaching (incorrectly) that articulating paper marks indicate occlusal contact force intensity based on the size, shape and color intensity of ink markings left on contacting teeth by the articulating paper. In theory darker and larger paper marks should indicate higher force, smaller paper marks should indicate lighter force, and the “bullseye” ink mark forms when excessive force is applied to a tooth surface removing some ink from the center of the mark. These concepts are echoed in a number of occlusion book publications.1–6
Sadly, it seems dentistry has ignored its own evidence-based literature, in which articulating paper mark studies clearly prove that a large paper mark indicates a forceful contact only 14% of the time, and that no correlation exists between mark size and applied occlusal load.7,8 In one study the inverse of the above theory was found, in that as applied bite forces to articulated casts were doubled and tripled, the paper mark sizes declined in size rather than increased.8 In short, as the applied load went up, the ink marks went down in size.
Furthermore, other studies indicate that static dental materials (foil, articulating paper/ribbon, ink impregnated strips, wax, or silicone imprints) have not demonstrated the capability to quantify occlusal forces, to detect occlusal contact time sequencing, or detect force transmission around the dental arch that occurs during a mandibular closure into Maximum Intercuspation (MIP).9,10 Articulating marks specifically only indicate occlusal contact location; not occlusal force levels and contact timing durations.7,11 Most importantly, despite that it is still taught that mark size describes occlusal force, the literature offers no evidence to suggest that variable articulation paper mark sizes can describe varying occlusal contact forces in any predictable way.7,8,11–13
What is of significant concern is dentist practitioners have been shown in two separate studies to be incapable of correctly distinguishing forceful from non-forceful occlusal contacts using articulating paper markings as the “force level” guide. These first-ever analyses of Articulating Paper Mark Subjective Interpretation, reported the 400 study participants chose correct forceful contacts only 12.8% -13.3% of the time.14,15 This means that the dentist-practitioners “Subjectively Interpreted” the wrong articulating paper markings 87.7% - 88.2% of the time. Importantly, no publication refutes these findings. In a recent anonymous polling study, a full 24% of dentists admitted to not treating occlusal disease.15 No doubt, their reliance on the analogue occlusal indicators have confounded their willingness to address patient occlusal problems.
Some dentists combine articulating paper markings with Shim-stock foil. But Shim-stock use also involves a great deal of dentist subjectivity.12 The advocated method to locate zones of forceful occlusal contact, is to place the foil between occluding teeth and then ask the patient to “close and hold” their teeth firmly intercuspated. Next, the dentist attempts to pull the foil out buccally from between the occluding teeth, while simultaneously “judging” how firmly the occluding contacts resist the foil from being removed.12 Studies indicate that removal forces from small occlusal spacing gaps showed no significant difference in Shim-stock contact “hold.”12,16 Also, because contact “hold” resistance levels are subjective, “hold” is a difficult guiding factor when selecting occlusal contacts for adjustment.17
Shim-stock is a non-quantifying occlusal indicator that has no force- measuring, force detection, or force reporting capability, nor does Shim-stock quantify occlusal contact timing durations. Also, because Shim-stock does not mark contacts on the selected teeth, articulating paper is still required to identify possible forceful contacts. Articulating paper then becomes the primary guide for selecting contact(s).17
Digital Occlusion
The era of Digital Occlusion began in 1984 when the T-Scan I technology revolutionized both dental occlusal science and daily clinical practice, by bringing objective precision measurement to the largely subjectively analyzed Dental Medicine discipline of Occlusion. The development of the T-Scan technology has required much iteration over the past 36 years beginning with T-Scan I, then T-Scan II for Windows®, then T-Scan III with Turbo recording, to a simplified desktop version introduced in T-Scan 8, to the present day version known as T-Scan 10, which costs approximately $11,995.00. Numerous authors since the mid1980s have studied the various T-Scan versions, which inspired the manufacturer to improve the hardware, and develop more accurate, repeatable, and precise recording sensors. These T-Scan system modifications aid a dentist in diagnosing and treating a wide range of occlusal abnormalities far more predictably than can be accomplished with articulating paper ink marks combined with Shim-stock hold.9,18
Multiple studies have validated the T-Scan sensor’s occlusal force reproduction and its timing quantification.9,19–26 Also, both a reliable recording methodology and definitive treatment protocols have been developed and tested in research environments. This has made it possible for dentists to use T-Scan data predictably, and reliably.27–40 There are presently 5 published volumes that describe all the researched TScan clinical applications in dental occlusal diagnosis, fixed and removable Prosthodontics, Implant supported & direct Prosthodontics, Periodontics, Orthodontics, Aesthetic Dentistry, Tooth Hypersensitivity to cold, Temporomandibular Disorders, and Mandibular Orthosis for Body Posture and Balance.19
Alternatively, Occlusense is a totally new digital occlusion product that was released in 2019 and costs between $1699 and $2400.00 from different distributors. It has no history of product development and improvement, nor has it been tested in research environments for its accuracy, repeatability, or validity as a patient treatment device. Occlusense must undergo academic scrutiny before it can be determined if it will be a useful clinical adjunct.
This Specific Aims of this manuscript are to compare in detail, both the T-Scan 10 and the Occlusense digital occlusal analysis devices, so that a non-owner reader can understand their inherent product capability differences, and how their differences impact each system’s clinical implementation.
HARDWARE COMPONENTS
OCCLUSENSE
Occlusense is a wireless digital system handle and sensor (Figure 1a) that transmits the data via a Wi-Fi connection, to an iPad Application. The patient’s recording is displayed on the App. The handle is wide and triangular to accommodate the wide shape of the sensor tab (the non-occluding extension that fits into the handle and mates with the handle electronics; Figure 1a).
The Occlusense handle has:
-
Control button 1 Pink - Start and stop a recording, and run the daily Function Test
-
Control button 2 Green – Initiate data transmission over Wi-Fi to the App.
-
A red charging LED - Indicates the handle is charged/not charged
-
An LED display window - Displays set up, Wi-Fi connection, and recording instructions, and displays a progress bar of the recorded data processing once a recording is completed.
-
A latch door – The top portion of the handle houses the LED display lifts open to replace sensors, and latches to hold the sensor in place during use
The Occlusense handle can record up to 0.056 seconds/frame of incremental digital occlusal data. It must be charged in advance to operate and will turn off after 4 minutes of inactivity.
To establish the technology is working properly, a daily handle Function Test is required, that employs a Test Sensor (Figure 1AB). The App will display a message as to whether the test passed. Once the function test is completed, the Occlusense handle can then record and transmit patient digital occlusal data to the iPad.
The Occlusense sensor is 60 microns thick. Its borders are anchored to a rigid cardboard frame that encases the metallic connection components of the sensor. The cardboard frame has no aid for consistently positioning the sensor in a patient’s mouth (Figure 1AB).
Both the intaglio surfaces of the sensor are coated with red articulating ink, to mark the teeth at the same time a digital data recording is being made. The inclusion of cardboard in the sensor design limits sensor use to 1 clinical session as indicated by manufacturer’s recommendation. These sensors that come with the purchase are one size, however a larger size may be ordered which is 6 mm wider. (order No. BK 5035).
Presently, there are no durability, repeatability, or accuracy studies about the Occlusense sensor, as it has not yet to date, been tested for its attributes or its capabilities in any published study.
T-Scan 10
The T-Scan 10 recording hardware components include the Novus recording handle, 2 sizes of plastic molded sensor supports and 2 sizes of the High Definition (HD) Novus-specific sensors (Figure 2AB).
The Novus recording handpiece (Figure 2AB) is the 4th generation T-Scan system recording handle. The Novus is ergonomically shaped to fit comfortably in a dentist’s hand and is equipped with a number of operational buttons that assist in recording and data playback, without the dentist having to navigate between the patient and the computer.
-
Power On LED Indicator - A green light that indicates the handpiece is powered on.
-
Sensor OK LED Indicator - A 2nd green light that indicates the Novus sensor is correctly seated and will record data
-
Sensitivity +/- Buttons - These 2 buttons increase or decrease the amount of electricity that charges the sensor to match the sensor response to the patient’s occlusal strength.
-
The Red Record Button - A multifunction button that opens a new scan, commences a recording, or stops a recording.
-
The Scan Mode LED Indicator - A green light that indicates the sensor is scanning force data and transferring that data to the computer.
The Novus handpiece can record up to 0.003 second incremental relative occlusal contact force and timing data when in Turbo Mode. It requires no charging, no daily Function Test, and is ready to use when connected to a computer via a USB cable. The cable connection allows for a high rate of sensor data transfer to the software and gives the dentist the ability to see the recording evolve during real-time recording.
The Sensor Support arms stabilize the sensor when it is clenched into and excursed upon, while its anterior positioning stabilizer aids the dentist or auxiliary in repeatedly positioning the sensor between a patient’s two maxillary Central Incisors (Figure 2AB). Sensor positioning ensures there is consistent contact force/tooth location capture, making contact force data mapping clinically reliable during data analysis, diagnosis, and treatment (Figure 2C).
The Novus HD recording sensor is 100 microns thick. It is a resistive, electronic tactile sensor that contains pressure-sensitive conductive ink distributed in columns and rows that are encased in Mylar, formed in the shape of a dental arch (Figure 2d).20 The sensor is not coated with articulating ink, is impervious to saliva, and can be alcohol-cleaned and reused on the same patient Figure 2 at subsequent visits. The HD recording sensor has been shown in studies to maintain its integrity for up to 24 uses and reproduce 256 occlusal force levels 95% of the time.9,20 Further, there are multiple published T-Scan sensor studies demonstrating that T-Scan sensors can reliably time-quantify occlusal contact sequences, and repeatedly report the relative force levels.21–26
PERFORMANCE CAPABILITIES
T-Scan has a 36-year-long history, during which the T-Scan’s 10 differing software and hardware versions were tested, criticized, and improved.9,19–23,25,26,41–47 The current version, T-Scan 10, records 256 levels of relative occlusal force presented in a multiple spectrum of colors, while simultaneously registering the sequence of occlusal contacts in 0.003 second increments. The T-Scan system measures and reports on the:
-
Occlusal force distribution on individual teeth, in each arch-half, or by dentist selected quadrants
-
The presence of any time-early and rapid occlusal force contact increases that occur as closure forces evolve around the arch
-
Locations of areas of excessive occlusal contact force
-
The percentage of occlusal force present on each tooth in relation to the maximum force that is exerted upon all occluding teeth
-
The transition of force movement around the dental arch as more teeth engage in closure, or disengage in lateral excursive movements
The T-Scan also features Warning Alarms for occlusal over loading of implants, and when poor recordings are made. And the T-Scan can be synchronized with Electromyography software in real-time that measures up to 8 masticatory muscles (T-Scan 10/ BioEMG III, Tekscan, Inc., S. Boston, MA, USA; BioResearch Assoc., Milwaukee, WI, USA). These synchronized technologies offer the dentist a notable advantage when making an Occluso-muscular diagnosis, or when rendering DTR treatment with the ICAGD coronoplasty.27,29–36,48
Occlusense reports 256 levels of force with a 4color coded scheme (green/yellow /orange/red). This color gradient implies masticatory force distribution in the area evaluated. Also, relative pressure differences between pressure points is indicated by the height of the pixels. The color and height of the pixels indicate relative difference in contacts to adjacent contacts. No publications on clinical accuracy or effectiveness exist to date.
Practicing Digital Occlusion by using data to isolate problem occlusal contacts is very different from practicing Subjective Interpretation, which uses ink marking materials and subjectivity to isolate occlusal contacts. Despite that marking ink sits on the Occlusense sensor, Occlusense’s generated digital datasets must be first understood to determine how its digital occlusal data can be used clinically, absent of what its ink markings appear like on teeth. Of note is that nowhere in the Occlusense product manual, is it explained how to use Occlusense data to improve a problem occlusal condition. At present, because Occlusense data is not understood, there is no known method for a dentist to apply its data clinically on patients, to obtain a predictably improved occlusal outcome.
Figures 2E-2H detail the differing systems’ known physical recording and playback attributes and their known clinical use applications.
Device Validation Studies
Sensor Comparison
Figure 2E describes that T-Scan 10 has been tested for its sensor accuracy, relative force reproduction and the accuracy of its time quantification. Occlusense has not been tested, and therefore its accuracy and repeatability for clinical implementation is unknown. Importantly, the T-Scan 10 has an existing and defined device-guided occlusal adjusting method that has been validated in studies to obtain improved adjustment occlusal force and timing parameter end results over conventional non-digital occlusal adjusting.18,19
Figure 2F shows the cost per sensor and the number of known uses/recommended uses of each system’s sensors.
The T-Scan sensor is 100 microns thick that when used is compressed to within 60-80 microns and can be used for up to 24 times before replacement.20
Occlusense sensor is 60 microns thick and covered with red articulating ink. The Occlusense sensor has a matrix-style sensing region that is similar to the T-Scan sensor. The manufacturer recommends the Occlusense sensor be used for 1 treatment session, as it cannot be sterilized or cleaned antiseptically. To date, the number of crushes it can withstand and still output accurate data is an unknown.
There is a significant cost differential between the two system’s sensors. T-Scan sensors cost $6.00 each and can be used many times, while Occlusense sensors are $16.00 each, and can only be used in 1 clinical session for a few times. Plus, as the Occlusense sensor is repeatedly used, the ink coating degrades affecting the sensor’s ability to ink mark the same tooth contacts during successive recordings.
Research of the Proven Device Clinical Applications
Figure 2G illustrates that the T-Scan 10 has had numerous clinical applications developed and researched, that use both time and force as the treatment guiding decision makers. T-Scan has known applications in many dental disciplines. Alternatively, Occlusense has none at the time of this comparison.
Recording Capabilities
Figure 2H details the various recording capabilities each system demonstrates. A definitive drawback of Occlusense is that although a dentist can live-preview a recording on the App screen, the live preview data cannot be recorded.
The actual Occlusense recordings cannot be viewed as they occur in real-time, to see if the patient moved correctly while the recording was being made, or if the data gathered from the patient was well or poorly recorded. And, before a recording can be played back to determine it was a useful data set, the handle must process and transmit the recording to the App, which manipulates the pressure gradient data to fit the Occlusense standardized dental arch outline (which has no individual tooth delineations). This lack of real-time recording means chair time must be utilized to find out if a recording can be used to analyze the occlusion, or if another recording is needed.
Alternatively, T-Scan is recorded in real-time, during which the dentist can watch the entire recording as it takes place, and can help the patient improve their mandibular movement, if need be, through mid-recording verbal coaching.48 The dentist can see the recording evolve, see the patient close or excurse correctly (or not), and see whether the recording was well-obtained from the patient. When visualizing a bad movement mid-recording, a TScan user can abort, and quickly pull up a new recording, and re-record a good quality recording, without having to wait through play back of the recording only to find out that a recording is flawed.
Playback Capabilities
After recording, the T-Scan data is not manipulated to fit a standardized dental arch when presented to the dentist. The T-Scan dental arch is customizable and can be properly set up to match the patient presentation. This arch customization can include incorporating digital scans (file format *.stl) of a patient’s maxillary and mandibular arches into the T-Scan 2D playback window (Figure 3). The T-Scan data is superimposed over the digital arch scan, simplifying the matching of force zones with the actual occlusal contact locations, intraorally.
In Figure 3 the T-Scan 10 playback desktop includes a maxillary arch digital scan overlaid with color coded force data sitting on the cuspal inclines and fossae of the involved teeth. This greatly simplifies determining any problematic contact locations compared to using Occlusense’s standardized arch outline.
Alternatively, the recorded Occlusense data is software-sized to fit within the standardized arch form that has no specific tooth delineations. The Occlusense arch cannot be altered to match the patient presentation. (Figure 4A)
Figure 4B details the various force quantifying tools that each system has, that help a dentist make an accurate force profile occlusal diagnosis. In addition to its 2D and 3D playback windows, the T-Scan has many software tools that aid in detecting where excessive relative occlusal force is present on a single tooth, in a quadrant, in both the right and left arch halves, and how force moves around the dental arch. With the T-Scan’s
Relative Force Quantification Tools
18-color scheme describing 256 force levels, the force level jumps from color-to-color are small, at 14 force levels/color.
T-Scan 10 FORCE TOOLS
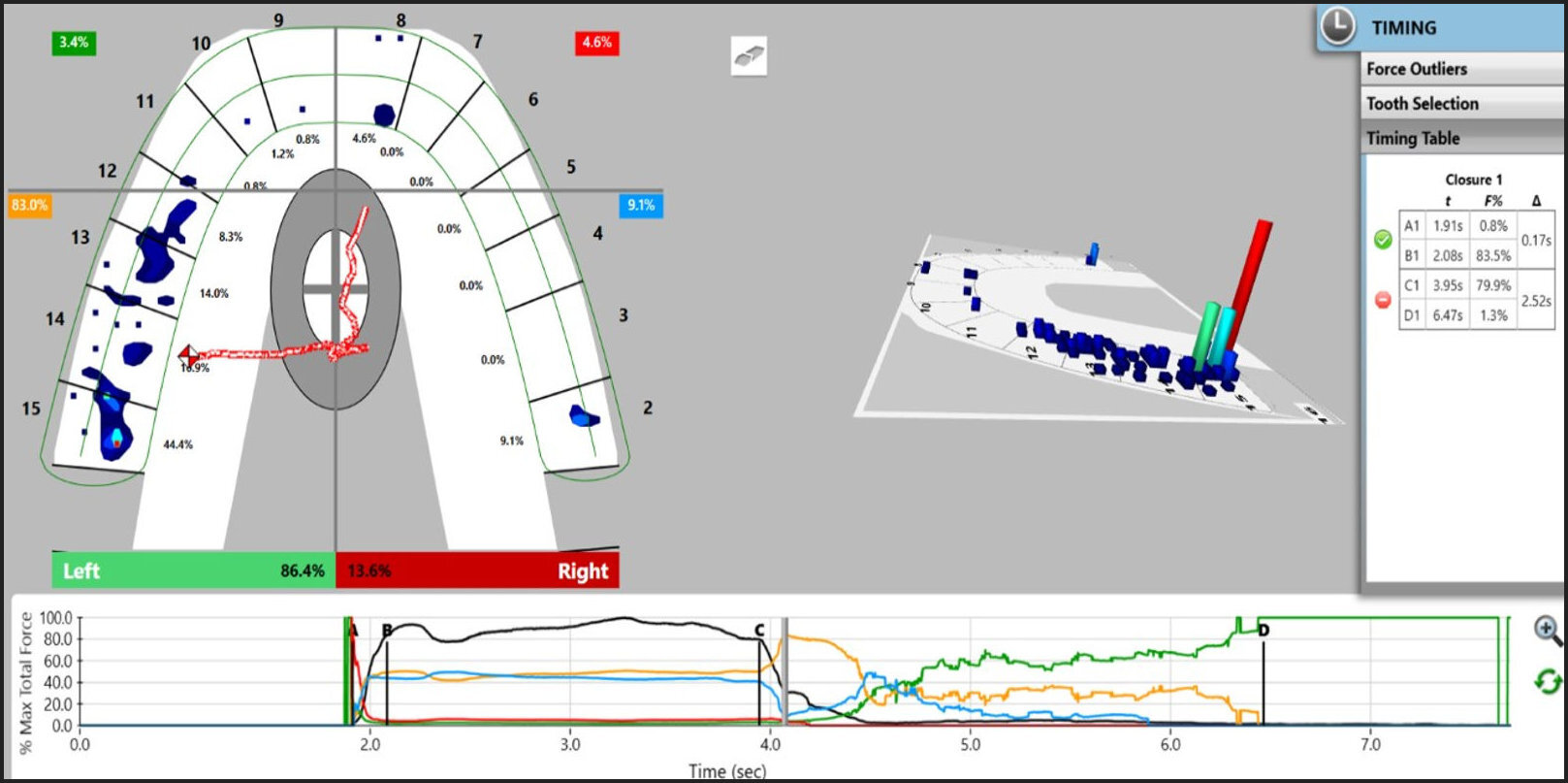
Two key T-Scan Force quantification tools are the Center of Force Target and Trajectory, and the Force vs. Time Graph (Figures 2c, 3, and 5).
The Center of Force Target and Trajectory tracks the history of changing total occlusal force summation positionally throughout contacting dental arches. The red and white diamond-shaped icon and its’ red colored-line trailer move towards higher force concentrations and away from lesser concentrations within the 2-Dimensional T-Scan data.
The COF marker pinpoints the location of the sum of the total force of the medio-lateral and antero-posterior force levels of all recorded occlusal contacts.
The Force vs. Time Graph describes a functional mandibular movement recording for the entire duration of that recording. The changes in Total Force during closure, the right side-to left side occlusal balance, and the force changes during excursive movements, are all illustrated by colored lines. The form of the black Total Force line illustrates the patient’s capability to make mandibular movements. The Force vs. Time graph also helps a dentist to know the recorded data is useful clinically, or whether a new and better recording is needed. (Figure 5)
Occlusense does not have these key Force Quantification tools but does present force in a similar 2 and 3 Dimensional windows as does the T-Scan.
OCCLUSENSE FORCE TOOLS
Occlusense uses its various App desktop displays to present the recorded occlusal pressure distribution to the dentist. The App desktop has both a 2D Force Snapshot view and a rotating 3D columnar view (very much like the T-Scan desktop), however the Occlusense 2D dental arch has no distinct individual tooth delineations that are correctible to match the patients true arch.
Relative pressure gradients (manufacturer’s term from the Occlusense manual) are depicted in the 2D Force Snapshot window by neighboring green, yellow, orange, and red colored data blocks, that change in color as the pressure distribution changes in different areas of the arch (Figure 6A). Small surface area contacts (pinpoint contact) are denoted by orange and red, whereas large surface area contacts (broad contact) are denoted by green and yellow. In the 3D rotational window, the same colored blocks are represented as columns with differing heights. With the Occlusense 4-color scheme describing 256 force levels, the force jumps from color-to-color are large, at 64 force levels/color.
The Occlusense App desktop has both a 2D Force Snapshot view and a rotating 3D Columnar view. In the 2D view, neighboring relative pressure gradients are illustrated by green, yellow, orange and red colored data blocks. Their matching variable height columns are located also on the arch model in the 3D view. See Figure 6a.
The force distribution can be presented to the dentist as an estimated force % / stock arch tooth. (Figure 6B) This display segments the perimeter of the stock arch, and then calculates the force percentage located in each segment. Because the stock arch is not matched to the patient’s true anatomical dental arch, this display option can only estimate the force % per tooth.
The 2D desktop can be segmented to estimate force % per stock dental arch tooth. And the sensor can be quartered into areas of relative pressure. The most pressure in this scan is the posterior left quadrant (solid red background), while the 3 other quadrants are comprised of similar pressure (solid green background).
Quartering the sensor, displays behind the Occlusense arch solid-colored regions of red (most pressure in quadrant), yellow (medium pressure in quadrant), and green (lowest pressure in quadrant), thereby grading each quarter’s force distribution. In Figure 6B, the most pressure is distributed in the posterior left quarter (solid red background), while the 3 other quarters all demonstrate similar amounts of pressure (solid green background).
However, no calculations of the numerical force % per arch-half or quadrant are presented to the dentist on the desktop. This lack of the arch-half, and right side-to-left side force % calculation, means Occlusense does not report to a dentist quantitatively, how imbalanced an occlusion or a dental prosthesis is.
Time Quantification Tools
Figure 6C details the various time analysis tools that each system offers a dentist that helps that dentist to make an accurate time-based occlusal diagnosis.
T-Scan 10
T-Scan 10 has numerous, published, time-based treatment protocols, that utilize the Timing tools within the software to quantify tooth contact time-sequence duration and order, isolate time premature contacts, and help visualize prolonged frictional excursive contacts.24–37,39,40
Calculating and reporting on both the Occlusion Time (OT) and the Disclusion Time (DT), are accomplished using the Force vs. Time Graph and the Timing table, which grades the physiologic health of these 2 important occlusal contact timing parameters. Within the Force vs. Time Graph, any recorded functional mandibular movement can be broken into key Time-Regions that are defined by 4 vertical, moveable time position lines (A, B, C, D Lines; Figure 5). The Occlusion Time (OT) is calculated between the A-B lines, and the Disclusion Time (DT) is calculated between the C-D Lines. Complete MIP intercuspation is calculated between lines B and C. In a properly recorded T-Scan data set (Figure 5), the distances between pairs of these lines horizontally, describes the contact timing duration of 1st contact into complete intercuspation (A-B; the OT), and excursive posterior disclusion until only the anterior guidance surfaces are in contact (C-D; the DT). The timing pane shows the values of the OT and DT and warns the dentist if the values are prolonged and non-physiologic (Figure 5).
OCCLUSENSE
Occlusense does not have and timing tools or time quantification capabilities. Occlusense however, does record dynamically the temporal sequence of intercuspation, which can be played back continuously, or incrementally frame-by frame, forwards and backwards. There is a Time Bar placed above the playback buttons, which shows playback progress of the patient’s occlusal video (Figures 6A & 6B).
Occlusense has no ability to qualify the physiologic health of the time-duration required by a patient to complete their temporal sequence of intercuspation. Absent is the quantification of key Time-Regions that occur during a functional mandibular movement. Therefore, no OT or DT can be determined without the dentist performing a manual calculation, by playing back a recording and marking the distance between certain timepoints.
A lack of time quantification and of key time-region duration calculation, are serious drawbacks of the Occlusense system, because a major component of practicing Digital Occlusion is to isolate problematic prolonged time-sequences in both closure (OT) and excursive movements (DT). Time-based occlusal adjusting optimizes the poor initial timing durations, which have been shown in many studies to dramatically improve Occluso-muscular physiology.24–37 Without time quantification capability, many routine patient T-Scan clinical procedures cannot be performed using Occlusense.
Raw Data Output Possible for Research
Figure 6D denotes that the T-Scan raw data can be exported for research analyses and computation in ASC II format. The “raw data” is the electronic Digital Output (DO) that changes within the sensor matrix during force loading and unloading of the sensor. T-Scan patient movie files can also be exported in their original form (*.fsx file), as .mov files to be played as a video, and as a complete patient file containing their customized arch form with all their recorded movie files (*.tpmc file).
Occlusense recordings can be exported using iTunes as a video file, and as images in *.png format, or as a pdf files. But the saved files can only be played within the iPad App. And unfortunately, Occlusense raw sensor electrical data cannot be exported for study or research.
METHOD of CLINICAL COMPARISON
The purpose of the evaluation was to review the efficacy and ease of use of both systems, as well as to compare the data findings/results from both systems to each other. T-Scan and Occlusense were each used to record five patient occlusions in Maximum Intercuspation (MIP), and right and left lateral excursive movements. Each recording per system was made once, and all of the recordings per patient were made with new sensors. Because Occlusense has no known and verified recording protocol, the known T-Scan recording method was employed with both systems. The occlusal recordings were evaluated at different time moments within each recording and evaluated for consistency of the recorded occlusal force profiles.
After completing the recordings, the data from each system per case, was compared, and the ink transfer from the Occlusense sensor was compared to the ink transfer from Accufilm 23-micron thick articulating strips (Parkell Inc., Farmingdale, NY, USA). Photos were taken of the patient’s arch after being marked with the ink coated Occlusense sensor and with Accufilm (since the T-Scan sensor is not coated with ink).
The data collected was not used to treat any case, but was gathered in a diagnostic manner and then compared from system to system. While there were some similarities between T-Scan and Occlusense data sets, T-Scan exhibited more pinpoint accuracy in locating individual high force contacts and excursive interferences. TScan reports relative occlusal force levels on individual teeth, while Occlusense reports broad zones of digital data rather than specific tooth locations.
The recordings overall, took less time with TScan, as it is a USB plug and play technology. Occlusense had to be paired to the iPad before a recording could be made, and then the data had to transfer from the recording handle to the iPad before it could be viewed and interpreted. During the evaluation, none of the T-Scan sensors perforated, but 3 Occlusense sensors did perforate in their first three uses. The thinner sensor no doubt contributed to the three perforations observed with the Occlusense sensor.
The total cost of the sensors used to make the recordings for each of the 5 cases were:
-
T-Scan – 5 sensors @ $6/sensor = $30.00
-
Occlusense – 9 sensors @ $16/sensor = $144.00
A thinner sensor might be more advantageous, as there would be less sensor material to interfere how teeth naturally come together. However, a thinner sensor comes with a failure cost because it is more easily damaged. It is important to note, no occlusal adjustments were made which means all occluding surfaces were smooth and not rough, which could have led to more perforations of both sensor systems.
The author looked forward to using the Occlusense system, since their sensors are coated with ink that would leave marks on the teeth at the same time a digital occlusal data recording was being made. Conceivably this would be a time saving feature, in that one does not have to use the sensor and the articulating paper separately (as with T-Scan), thereby essentially saving a step. Unfortunately, this concept did not meet my expectations, nor did the execution actually succeed. Figure 7d shows much less ink was transferred to the teeth following recording with the Occlusense sensor, when compared to the Accufilm articulating paper markings seen in Figure 7b. More importantly, the ink transfer to the teeth from the Occlusense sensor did not match the Occlusense data or the T-Scan data, as shown in Cases 1 and 2 (Figures 7A-D; 8A-D).
RESULTS of CLINICAL TESTING
In the following case comparison examples, all 2Dimensional T-Scan data sets were aligned to match the orientation of the clinical pictures (the patient’s right ach half is on left side of the clinical picture, and the right T-Scan data is on the left side of the 2D T-Scan window). Each TScan 3-Dimemsional column window was aligned to match its comparison Occlusense 3Dimemsional column window.
Case 1 is described in detail within Figures 7A-D
Figure 7A is case one T-Scan data of Maximum Intercuspation (MIP), showing teeth #2 and #7 have the greatest amount of, and highest intensity contact forces, with 35.8% of the total bite force located on tooth #2. There is a light-force contact on tooth #8, and no occlusal contacts visible on teeth # 9 and 10. Most importantly, the T-Scan has calculated an 85.8% right-14.2% left occlusal force imbalance, with the COF Icon and trajectory located on teeth #s 2-4 throughout the entire closure into MIP.
Figure 7B is Occlusense data of the same patient in MIP showing more high force columns (than did T-Scan) of the same height and color intensity distributed around the arch. Also, Occlusense reported occlusal contacts of severity exist anteriorly, where T-Scan reported low force or no contact. Since the Occlusense sensor does not discriminate force levels as well as does the TScan HD sensor, it reported some false positive occlusal contacts.
A very important chairside Occlusense use problem is illustrated in Figure 7B. Occlusense placed 32% total bite force on tooth #3 and 4% on tooth #2. But, T-Scan showed 38.5% of the total bite force is on tooth #2; not tooth #3. Because the Occlusense arch cannot be changed to match the patient’s missing teeth, it can place occlusal forces on the wrong teeth from where those high forces actually exist, intraorally. This non-modifiable arch problem definitely complicates the dentist’s determination of where is the exact contact that contains the highest bite force. In this example, Occlusense clearly placed the most bite force on the wrong tooth.
Figure 7C shows the Accufilm Ink marks that are correlated to Figure 7a with high force on teeth #2 and #7. The Accufilm articulation strips transfer ink more effectively than does the Occlusense sensor (See Figure 7D).
In Figure 7D significantly less ink was transferred to the teeth from the Occlusense sensor than was transferred with the Accufilm (Figure 7C). A different formulation of ink may be required for the marking ink to adhere to the sensor that affected the ink transfer. Or perhaps the rigidity of the sensor interferes with good ink transfer onto the teeth. A lack of appropriate ink left on the teeth can deny the operator the opportunity to make the correct adjustment.
Case 2 is described in detail within Figures 8A – 8D.
Figure 8A is the T-Scan data of a Left Lateral Excursion with the T-Scan arch corrected with edentulous spaces that match the patient’s dental arch. (Figure 8C) Both working and non-working interferences were recorded early in this excursion to the left. The T-Scan force data is presented to the dentist with 18 color-coded varying force levels displayed all throughout the arch.
Figure 8B is the Occlusense data in a Left Lateral Excursion, again with an arch that cannot be corrected to match the patient’s arch. The Occlusense force data does not sit on the same teeth as where the forces are located on the patient’s teeth, making it difficult for the dentist to know where corrective adjustments should be made. Also, the Occlusense reported that the 1 non-working and 3 working interferences all contained the same amount of force, displayed as tall red/brown columns.
Figure 8C shows the Accufilm markings of the left lateral Excursion made from MIP that correlates with T-Scan data from Figure 8A. Adequate ink transfer illustrates the degree of excursive interferences present on the involved teeth, which correlates well to the T-Scan data in Figure 8A.
In Figure 8B at this moment in the Occlusense data, tooth #14 has 47% of the total bite force, with no force percentage present on the anterior teeth. The “Show Quartered Force Distribution” suggests the anterior left quarter has higher total force than the posterior left (being designated in yellow with the posterior left quarter being designated in green). However, the anterior left quadrant only contains 29% total force, while tooth #14 has more total bite force (47%) than is present in the entire anterior left quarter. This quartered view incorrectly labels the posterior quarter as having less force (incorrectly labeled as green), than does the anterior left quarter (incorrectly labeled as yellow).
Case 3 is described in detail within Figures 9a-e
Figure 9A is another Left Lateral Excursion recorded by the T-Scan showing the COF traveling to be posterior left as the excursion evolves. This indicates forces go up the posterior left teeth when the patient moves laterally. In the Force vs. Time graph this is denoted by the orange quadrant line rising and controlling the excursion.
Figure 9B is a Left Lateral Excursion made by the same patient recorded by the Occlusense. Here is another dental arch where Occlusense cannot match the patient’s presentation in that teeth #s5 and #12 do not exist in this patient’s occlusion, shortening the arch by 2 teeth (Figures 9c and d). Occlusense graded missing tooth #12 as containing very high force (22% of the total force). T-Scan alternatively graded teeth #s 11 and 13 (which could be #12 in Occlusense) with only 6% of Total Force (Figure 9A).
Figure 9C shows the upper arch marked with Occlusense red ink, with better ink transfer than was seen in Cases 1 and 2.
Figure 9D shows the upper arch marked with blue Accufilm, which transferred more ink onto the teeth (than did Occlusense) that are involved in the left excursion.
In Figures 9A & 9B, both systems recorded similar working and non-working interferences midway thru the excursive movement, although T-Scan detected many differing force levels contained within those interferences, and more clearly represented those differing force levels to the dentist (Figure 9A). Occlusense reported most of the working side interfering contacts as being high force (Figure 9B). Alternatively, T-Scan recorded a working interference on tooth #15 with over 50% of the Total force but graded low force concentrations on teeth #s 11 and 13. Occlusense recorded #14 with over 50% of the Total Force, which is very dissimilar to T-Scan (#14 contains only 5% of Total Force in the TScan data). In Occlusense #14 displayed 54% of the total bite force, with that posterior left quadrant designated in yellow, indicating it is a moderately high force quarter.
Figure 9B is another example of how the Occlusense sensor surface is too sensitive to electronically grade distinct occlusal force levels. Occlusense shows all the lateral interferences as being high force. However, the T-Scan HD sensor can be software-controlled to mute its electronic sensor response when recording, detecting, and displaying multiple levels of graded forces. This helps the dentist isolate the truly problematic high force contacts when making a diagnosis or rendering treatment. Marking effectiveness of red Vs blue ink is shown in Figures 9C & 9D.
In Figure 9E, later in the same excursion, Occlusense tooth #15 matches T-Scan tooth #15, equaling 51% of the Total Force. Unfortunately, Occlusense also records 49% on tooth #14, which only occludes with 5% Total Force in the corresponding T-Scan data. At this time-moment within the excursion, even though the threshold slider was used to attempt to adjust the sensitivity, Occlusense did not detect any non-working interference on tooth #2.
CASE 4 is described in detail in Figures 10a-e.
Figure 10A is an MIP Scan made with Occlusense. Note the broad blocks of force that the sensor reports (blue box outlines). This block force representation makes individual contact force determination quite difficult.
Figure 10B is an MIP Scan of same patient made by T-Scan. Notice the T-Scan data has 12.0% of total bite force on tooth #15 and 13.4% on #14. While Occlusense has 27% on tooth #15 and 18% on #14. Both Occlusense and T-Scan show low force occlusal contacts all through the anterior teeth.
Comparing these 2 data sets, the actual force distribution on each individual tooth is more defined in the T-Scan. With Occlusense it will be more difficult for a dentist to locate the actual highest force, which is on the distobuccal of tooth #2 and distal of #15 (Figure 10A pink columns). However, Occlusense reported #2 distobuccal and the distal marginal ridge of tooth #15 as only being moderate force (green and light green columns).
Also observe how wide buccolingually and tall mesiodistally were the activated areas of the Occlusense sensor (Figure 10A, top pane; blue rectangular outline boxes). The block shapes that define the pressure distribution in the posterior areas really showed that sensor response.
In this way, the T-Scan colored force zones are far more representative of where and where the entire tooth width and dimensions were being activated from opposing occlusal surface proximity. The Occlusense sensor surface activation encases the occlusal contacts somewhere within those large rectangular sensor regions. Occlusense is unable to discern and separate the actual occlusal contact force levels, from when the sensor surface approximates nearby tooth surface, but does not make actual tooth contact. The sensor, therefore, is reporting force data that is not limited to occlusal contact.
Alternatively, note that the T-Scan force zones (made from the same patient intercuspating into a T-Scan sensor), are contoured and not blocky. The T-Scan sensor is less active at its surface because it can be electronically limited by the T-Scan’s software Sensitivity Setting. Tooth surface approximation to the T-Scan sensor surface does not activate a significant untoward sensor response.
At the perimeter of the Occlusense posterior tooth data, which is on the activated sensor surface where there is no contact, there are moderately forceful contacts being displayed (yellow and greens columns). Alternatively, at the perimeter of the T-Scan force zones there is mostly low force (dark blue, short columns). This is logical because occlusal force spreads out from the contact point where it would be highest, becoming lowest at the periphery of the force spread.
This case also re-illustrates that T-Scan detects and displays the differing force levels color-wise, more clearly than does Occlusense. T-Scan grades force differences in much smaller jumps from level to level than does Occlusense. Figure 10A showed that the T-Scan sensor records the forces with far better individual contact force level distinction, while the Occlusense sensor cannot selectively activate where the actual occlusal contacts occurred.
A filter can be applied to the Occlusense Data (Figure 10c), which removes differing force levels from the displayed force data. However, it does not alter what is recorded, and only removes visible forces from the data display. In Figure 10c, the filter helped remove the higher force data from the posterior areas (much of the red/brown column data was removed), but the Occlusense data maintained its block force shapes, displaying a less wide zone of moderate intensity force (green columns). The filter did not (in this example) help the dentist find the true high force contacts (#2 distobuccal and the distal fossa of tooth #15).
Figure 10d shows the Ink marks from the Occlusense data shown in Figure 10a, barely labeling the teeth and restorations with marking ink. This very little ink in no way matches the broad block areas of force data seen in Figure 10a. While Occlusense indicates 48% of total bite force is present on teeth #2 and #3, there is very little ink transfer visible.
Figure 10E shows the ink marks made from Accufilm used with the T-Scan recording Figure 10b. Accufilm transfers significant ink onto the occluding surfaces of teeth #s 2 and 3, where T-Scan indicates there is 31.1% of the total force.
Case 5 is described in Figures 11A – 11C.
Figure 11A is a side-by-side comparison of ink markings showing a similar distribution of Occlusense (left pane; red ink) and Accufilm (right pane; blue ink). Tooth #2 is missing and should be represented as such in both data sets, but the Occlusense arch cannot accommodate the removal of missing teeth.
Figure 11B is the T-Scan data of an MIP closure. Notice how #2 is missing in Figure 11A and the TScan arch can be altered to match the patient’s presentation.
Figure 11C is the Occlusense data of the same patient’s MIP closure. Occlusense indicates higher forces exist in the anterior (tall red columns) when there are no anterior high force contacts present in the T-Scan data. Five years ago, following a motor vehicle accident, the author rebuilt an existing anterior bridge that has been followed in the practice, and has had yearly occlusal evaluations to ensure the bridge was not overloaded. So Occlusense is over reporting force levels once again, in Case 5. Also, worth noting is in the area of #2-31. The Occlusense data displays 3 red small columns when there should be no contact because tooth #2 is missing. It is also not clear as to why there are small red columns and tall red columns in the same data set.
Sensor Durability During Comparison Testing
In this side-by-side comparison on the five test cases, Occlusense sensors perforated frequently, rendering them useless and requiring replacement. This occurred with 3 repeated crushes of the Occlusense sensor in MIP (Maximum Intercuspation), and when the patients made left excursive movements. However, none of the T-Scan sensors perforated at any time during the comparison.
It appears that the thinner Occlusense sensor did not withstand the repetitive forces applied from the teeth, as there is 25% less material between the teeth than there is with a T-Scan sensor. However, if the Occlusense sensor frequently perforates, it will greatly interfere with chairside clinical use of that technology.
Concept of Appropriate Sensor Thickness
A hole or perforation in a strip of film, foil, or marking paper does not interfere with process of marking teeth, other than there may be no ink on the strip to mark an actual contact. However, a perforation in a digital sensor creates an electronic failure that corrupts the force and timing data. As such, digital sensor durability is essential, so that a sensor’s structure stays intact while being repeatedly crushed inter-occlusally during the recording process. Sensor integrity ensures the dentist is able to record useful and reliable patient digital occlusal force and timing data.
Sensor “thickness” then becomes a positive physical attribute, in that appropriate material dimensions can both withstand the stresses of occlusion, and repeatedly, reliably report consistent force and time values, without sustaining frequent perforations. Surface tooth roughness, restorative material graininess, porcelain chipped edges, and metallic occlusal surface anatomical indentations, can perforate a sensor substrate, which creates then a clinical problem for the dentist, who must change sensors frequently, smooth the roughened area that caused the perforation, and then re-record the perforated data. These recording failures then interfere with patient flow during a computer guided occlusal adjustment procedure.
The T-Scan sensor has been consistently criticized for it being considered “thick”. And yet it in this comparison, it held up far better than did the thinner Occlusense sensor, while recording consistently without perforating. The T-Scan HD sensor Mylar matrix has been shown in studies to maintain its integrity and reproduce force output and time data, consistently.9,20–26,28 Therefore, it’s 100-micron thickness prevents frequent perforations. Further, despite all the TScan cited literature in this paper’s Reference list, no T-Scan author has reported “frequent sensor perforation” as being a consistent problem when recording with different T-Scan sensor generations. One study that tested many occlusal indicator materials (T-Scan sensor, articulating paper, foil, silk ribbon, wax, and silicone imprints), reported the T-Scan sensor was the only material capable of reproducing the test environment 18 out of 19 times.21 It appears now that a thinner sensor has been developed for recording digital occlusal data (Occlusense sensor), a sensor thickness that resists matrix breakdown is required to gather useful digital occlusal data.
DISCUSSION
Author’s Impression After Clinical Comparison of 5 Patients Recorded by Both T-Scan 10 and Occlusense
I purchased an Occlusense based on two main selling points I thought Bausch had capitalized on. The first was Occlusense is a wireless system. The second was the sensor was coated with ink to mark the teeth where force contact in the data could easily be matched to the ink on the teeth. My experience after using the Occlusense for the past few months has left me less than enthused.
One of the biggest Occlusense frustrations was that the Wi-Fi connection lost its connectivity to the iPad with some regularity. This increased the recording time, as one must exit out of the software and reconnect the handle to the iPad, and then return to the Occlusense software. Unfortunately, this occurred multiple times with each patient during the testing and would likely be a frequent problem that would interfere with rendering occlusal adjustments.
Another difficulty using Occlusense to record, was that the cardboard encased sensor has no intraoral sensor stabilizing elements. This makes it challenging to place the Occlusense sensor into the mouth, without it folding up, or without marking ink rubbing off onto the teeth, leaving pseudo/false markings. However, T-Scan sensors sit inside a sensor support, which contains a prong that rests within the mid-incisal embrasure that stabilizes the recording handle and sensor when gathering data from the patient. Occlusense has no such sensor stabilizer to rest within the midline embrasure, which made getting repeatable data challenging, as the sensor can move during a patient closure.
Also, the ink transfer from the Occlusense sensor onto teeth is not what I have come to expect from Bausch. Having used their articulating paper in my practice, their conventional strips better transfer ink to the teeth than does their sensor, perhaps because the sensor stiffness affects the quality of the ink mark formation. When a sensor is intercuspated into it crimps around the teeth, after which its data becomes more stable.20 That doesn’t necessarily mean the matrix of a sensor is ideal for transferring ink markings onto teeth, despite that it combines recording and marking in 1 step, that could theoretically lessen chair time.
In concept, these two Occlusense features seem like great advances that should have Tekscan nervous. However, the features did not perform as I had hoped. Occlusense should be quicker and easier to use in the sense one saves a step by having the sensor leave the ink on the tooth. But there is no way to correlate contact location to actual teeth before rendering an adjustment. No actual tooth locations or teeth identifiers exist that are accurate. The software has no tooth delineations, nor does the sensor, which made it challenging to correlate the data sets to anything clinical.
Alternatively, T-Scan allows the arch form to be adjusted to represent the tooth configuration the patient presents with. An example of this can be seen in Case 1 (Figures 7a-d) where tooth #5 is missing, and the arch was closed via orthodontic treatment. The T-Scan allows for more accurate data representation by making it possible to open or close spaces between the patient’s digital arch. In another case the patient presented with missing molars and a space between teeth #s 11 and 12, making the Occlusense standardized arch form and data unusable (Figure 8d). Most importantly, by having an unalterable standardized arch, areas of high occlusal force can appear on the wrong teeth in the Occlusense App.
Further, excursive movement recordings on the Occlusense are not diagnostic. Occlusense cannot distinguish differing levels of force very well, which is a huge drawback. In Figure 9a, T-Scan shows detected 4 contacts all with different levels of force, but Occlusense shows the same 4 contacts as being high force. The Occlusense data would guide a dentist to adjust every contact. As a result, the data is not useable to render corrective care. Moreover, Occlusense cannot be linked to an Electromyography system, nor can it quantify time, prohibiting its use in excursive therapy like Disclusion Time Reduction (DTR) with the ICAGD coronoplasty.48
The printed Occlusense manual was entirely in German, with no translations in any other language. The app did contain a PDF version in English but made switching back and forth from the manual to the app challenging on the iPad when learning the new technology.
Lastly, data management with Occlusense is a concern, because Occlusense data is not recorded to the office server, so automatic nightly back-ups do not occur. This creates extra data management steps as Occlusense data should be part of the patient record and must be maintained. Its data, however, can be stored in the iCloud or transferred individually for each patient at the end of the day or weekly, to the patient’s electronic chart to secure the data. I prefer to have all my data in one place with multiple back-ups. To accomplish this with Occlusense at the present time, requires extra steps to maintain all the data in one location. T-Scan is server based, so no matter which operatory computer is used, the database is saved on the server, and is accessible from any computer on the network.
CONCLSIONS
No known recording and clinical adjustment protocols, false positive contacts and high force representations when low forces were detected by T-Scan, the inability to correct the arch form to match the patient’s presentation, frequent sensor perforation, and an inability to quantify force accurately, leads this author to caution a potential purchaser. The author did read the manual and used it as the manufacturer recommended. While the two devices are vastly different in features and the one thing that should remain consistent in the comparison is the quantification of force. It is my opinion that they should be very similar in quantification of force. After all, 65 miles per hour should be the same in an SUV or in a motorcycle.
Conflict of Interest Statement
Dr Sutter is not a paid consultant for any dental equipment company or post graduate training facility.
Funding Statement
No funding was provided from any source for this review activity.
_occlusense_must_undergo_a_daily_function_test__to_establish_the_handle_is_working_pr.jpg)
_occlusense_must_undergo_a_daily_function_test__to_establish_the_handle_is_working_pr.jpg)














.jpg)

_the_accufilm_(parkell_inc.__farmingdale__ny__usa)_paper_marks_that_correlate_to_the_.jpeg)


_accufilm_blue_markings_of_the_left_lateral_excursion_made_from_mip_that_correlates_w.jpeg)


_upper_arch_marked_with_occlusense_red_ink__with_better_ink_transfer_than_was_seen_in.jpeg)



__but_with_the_vertical_filt.jpeg)
_ink_marks_from_occlusense_in__figure_10a_(156125)_were_barely_labeling_the_teeth_an.jpeg)


_occlusense_must_undergo_a_daily_function_test__to_establish_the_handle_is_working_pr.jpg)
_occlusense_must_undergo_a_daily_function_test__to_establish_the_handle_is_working_pr.jpg)













.jpg)

_the_accufilm_(parkell_inc.__farmingdale__ny__usa)_paper_marks_that_correlate_to_the_.jpeg)


_accufilm_blue_markings_of_the_left_lateral_excursion_made_from_mip_that_correlates_w.jpeg)


_upper_arch_marked_with_occlusense_red_ink__with_better_ink_transfer_than_was_seen_in.jpeg)



__but_with_the_vertical_filt.jpeg)
_ink_marks_from_occlusense_in__figure_10a_(156125)_were_barely_labeling_the_teeth_an.jpeg)


