INTRODUCTION
Exteroceptive suppression (ES), more commonly referred to as the EMG Silent Period (SP), can be seen as a brief cessation of recorded electro-myographic elevator muscle activity within a functional burst. Neurologically, it is a mono-synaptic nociceptive (protective) reflex locally initiated by a number of different stimuli.1,2 In addition to the short latency ES1, there is a polysynaptic long latency ES2, which is presumed mediated by afferents descending in the spinal trigeminal tract connecting with excitatory interneurons located in the reticular formation.3 A recent study claimed that age by itself changes the onset latency of ES1 and the appearance of ES2.4 However, this rather speculative conclusion was produced using artificial electrical stimuli and is suspect due to the difficulty of isolating just age effects from all of the other factors present.5
SP can be intentionally triggered by; a) tapping on the chin while a subject is biting,6 or b) by applying an electrical stimulus while biting.5,7 It can also naturally occur from a TMJ click of sufficient intensity as muscle spindles are excited by vibration or jaw jerk,6 or occur unintentionally due to a deflective tooth contact during normal mastication.8,9 The latter case is the objective of this investigation as it represents a primary irrefutable means of the detection of unavoidable occlusal contacts during chewing.10,11 Using an artificial stimulus to trigger the SP is useful if the purpose is just to evaluate the reflex, but measuring the SP during actual masticatory function reveals the presence of nociceptive reflex responses to any unwarranted occlusal contacts.
The ES1 Silent Period results from a monosynaptic nociceptive reflex locally triggered to protect the system when a tooth contact or hard artifact in food is encountered.1 Unlike the stable responses encountered when elicited under the carefully controlled conditions, during actual mastication ES1 responses vary depending on the a number of factors such as amount of muscular effort and strength of contact.12,13 A premature tooth contact is a common triggering mechanism occurring during mastication. With a brittle food bolus, SP occurs whenever a food bolus fractures suddenly.13
For very slight contacts the duration of the SP is terminated quickly. See Figure 1a. With a more substantial contact within the same chewing sequence a longer duration is seen. See Figure 1b. If the stimulus is strong enough, there is a contractive response applied to the depressor muscles to open the jaw,14–16 a flexor reflex just like touching a hot surface. This jaw opening reflex is the response seen when biting down on a pearl or more likely, a piece of shell when eating an oyster, which mechanically stimulates the teeth in both the upper and lower arches simultaneously.17 It has been proposed that frequent triggering of the SP tends to increase the duration the response in TMD patients.18 In fact, at one point in time an SP with a long duration was thought to be an indicator of TMD.19,20 However, while this relationship applies to TMD patients with painful muscular symptoms, it does not necessarily apply to all of those with primary internal derangements.
OBJECTIVE
This investigation compared the incidence and mean duration of measured Silent Periods within a TMD group during 15 cycles of masticating a consistent tough bolus to the same functional activity of an age and gender matched control group. The null hypothesis was: “No difference in the incidence or the duration of the measured silent periods between the control group and the TMD group.”
METHODS
Surface electromyography was used to record the activity from the bilateral superficial masseter and anterior temporalis muscles of 20 muscularly symptomatic TMD patients (37.2 +/- 17.55 years) after JVA and MRI verification of normal TMJ function (11 female). 20 asymptomatic age matched (p = 0.2739) and gender matched (11 F) control subjects (40.6 +/- 17.97 years) were also recorded following the identical protocol. A tough and reproducible bolus was provided to challenge the masticatory system and selected to represent a moderately difficult mastication task requiring at least 16 chewing cycles. Skipping cycle 1, cycles 2 through 16 were reviewed because cycle 1 usually contains excessive bolus manipulation. The number of Silent Periods present were counted and the duration of each one measured to the nearest millisecond.
The criteria for the TMD symptomatic group included muscular symptoms of any kind, but excluded TMJ noises or limitation in the range of opening. This was required to remove the possibility of TMJ precipitated Silent Periods. The control group was selected from fully asymptomatic subjects without regard to any aspect of the occlusion (Class I, II, III, overbite, overjet, etc.), but excluded the presence of a crossbite or missing and unreplaced molars or premolars except third molars. By selecting a moderately tough bolus each chewing sequence required more than 16 cycles to masticate the bolus completely. The tough bolus also created a sequence that gradually approached centric occlusion as the bolus was consumed.
Statistical Analysis
The Mann-Whitney U test was used to compare the mean age differences between groups as well as the median integer counts of the incidence of Silent Periods. Student’s t test for means with different variances was used to detect any significant difference in the mean Silent Period durations. Two examples of the appearance of suppression in Silent Periods are shown in Figure 1. (a = 0.05).
The TMD patients and control subjects were informed of all procedures, they gave their consent and the procedures followed the World Medical Association’s Declaration of Helsinki guidelines. Because this was a retrospective analysis of previously recorded data in a TMD clinic, an IRB exemption was obtained.
RESULTS
The median number of Silent Periods in the TMD group was 12 Silent Periods in 15 cycles and the comparable median number in the control group was 3 Silent Periods in 15 cycles (p < 0.00001). The TMD group mean duration of the Silent Period was 18.3 (+/- 8.31) milliseconds and the comparable number for the control group was 9.8 (+/- 4.23) milliseconds (p < 0.00001). The total number of SP among the female controls was 39 and the male controls 26, but because there were two more females than males, the adjusted equivalent female control score was 32. The total number of SP among the female TMD group was 120 and the male TMD group 117, but because there were 2 more females than males, the adjusted equivalent female score was 98. No significant gender difference was found in incidence. See Figure 2.
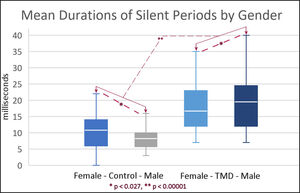
The mean duration of the silent periods of the females in the control group was 11.1 (+/- 4.96) milliseconds. The mean duration of the males was significantly smaller at 8.3 (+/- 3.17) milliseconds (p = 0.0264). The mean duration of the silent periods of the females in the TMD group was 17.0 (+/- 7.37) milliseconds. The mean duration of the silent periods of the males in the TMD group was significantly larger at 19.6 (+/- 9.01) milliseconds (p = 0.023). Gender differences are shown graphically in Figure 3.
To determine if the number of Silent Periods remained constant throughout the sequences, a comparison was made between the first 7 cycles and the last 7 cycles of all sequences to determine the total number of occurrences and their mean durations. For the TMD group the total number of occurrences of SP in the first 7 cycles was 108 and in the last 7 cycles 112, indicating a very constant rate of occurrence. The mean duration of SP was 18.4 (+/- 8.71) in the first 7 cycles and the mean duration of SP was 18.2 (+/- 8.10) in the last 7 cycles indicating no significant change (p = 0.8767).
For the control group the total number of occurrences in the first 7 cycles was 31 and the number in the last 7 cycles was 36 indicating a non-significant 16 % increase (p > 0.05). The SP mean duration in the first 7 cycles was 9.0 (+/- 3.47) milliseconds, increased to 10.6 (+/- 4.72) milliseconds in the last 7 cycles, indicating a trend towards an increase, but a non-significant one (p = 0.0685).
DISCUSSION
Exteroceptive suppression has been recorded in many studies, (e.g. already in the 1970s and 1980s), to evaluate the presence or the severity of “TMJ Syndrome” from the duration of an elicited Silent Period.19,21–23 Ultimately, some of the same authors that were promoting its use then, subsequently concluded that the silent period could not be useful to evaluate TMD.24 However, newer studies have revealed that the latency and duration of Silent Periods typically increase along with increasing incisal velocity, which increases the momentum at impact.13 Others have subsequently found that differences in many other parameters available from EMG data, such as resting activity, clenching activity, mean power frequency, asymmetric activity with symmetric functions, as well as the Silent Period duration, are most often significantly different within TMD patients’ EMG records.20
Within this study the Silent Period was not elicited but occurred randomly during the natural mastication of a tough, but not brittle bolus. The presence of Silent Periods was only considered as an indication of tooth contact during mastication because the bolus was one that did not fracture and all SP occurred within the chewing burst very close to occlusion. See Figure 4.
While there are other triggers for SP, they involve clicking TMJs and/or sudden muscle movements that were not exhibited within this study group. The strongest TMJ clicking is due to the reduction of a displaced disk that occurs during opening, when the elevators are relatively inactive and far less likely to produce a Silent Period. A closing click due to the TMJ disk displacing can produce a Silent Period, but not usually at or very near to occlusion as recorded during mastication. Within this TMD group, all TMJ internal derangement clicking was excluded.
Most of the subjects in the control group also produced a couple of silent periods, but the incidence was significantly less and durations significantly shorter than for the TMD group. In contrast, some of the subjects in the TMD group produced one or more Silent Periods within every cycle. See Figure 5.
The worst-case scenario is a TMD subject producing multiple SP within a single burst. This has been found previously in TMD subjects.25 This previous study detected significantly fewer Silent Periods during gum-chewing in a TMD group after occlusal adjustments that removed all of the contacts interfering with lateral excursions by exclusively using the T-Scan coronoplasty method of Immediate Complete Anterior Guidance Development (ICAGD), which reduces the time needed to disclude posterior contacts and is also referred to as Disclusion Time Reduction (DTR) therapy.
Gum is most often used for testing masticatory function because gum, compared to a tough bolus, produces a smaller number of incidences of SP in asymptomatic subjects25 and dysfunctional TMD patients can still chew gum, but not necessarily a tough bolus. This is especially true with TMD when an internal derangement is present. The duration of the SP within a chewing sequence is proportional to the strength of the tooth contact until a maximum duration is reached. A slight tooth contact produces a short, less distinct SP but a heavy tooth contact consistently produces the maximum duration SP. See figure 7.
However, gum-chewing also differs from the mastication of a food bolus in that it is not consumed and once it is softened, it is far more predictable than a challenging food bolus.26,27 In the mastication of a food bolus, the continuous changes in size, shape and texture all affect the process.28
The main advantage of testing with a tough bolus is that it challenges the masticatory system. Any subjects with only a marginal dysfunction can usually manage to chew gum with a reasonably normal pattern, but when attempting to masticate a tough bolus, the actual level of dysfunction is revealed. Even asymptomatic control subjects will increase their production of Silent Periods from an average of 0.5 SP/15 cycles with gum to about 3 SP/15 cycles when masticating a tough bolus.25 It is usually sufficient to record from the working side masseter to count the number of Silent Periods,11 although under some worst-case TMD conditions, the so-called working masseter is not working very much at all.
Except for the most fleeting of SPs occurring when only the slightest contact is made, most of the time the SP can be seen bilaterally in the EMG data of all of the elevator muscles. When it is not a clear suppression of all of the elevator muscles, the stimulus is just at the threshold level of triggering a response.
LIMITATIONS
The control group did not have their TMJs imaged with MRI for obvious economic reasons and their joint conditions were tested with JVA only. The main purpose of testing the control group was to assure that the TMJs were functionally normal. The specificity of JVA has been measured at 98 %, giving confidence to its ability in detecting normal TMJs.29 However, the complete category of Temporomandibular Disorders includes as many as 40 distinct conditions. This TMD group was restricted to patients with muscular symptoms, but without TMJ symptoms, for the purpose of limiting the number of variables. Since TMJ symptoms are the most common TMD symptoms, this exclusion makes extrapolation of this result to the whole of the TMD population limited.
CONCLUSIONS
The null hypothesis was rejected. In this group with muscular TMD symptoms, exteroceptive suppression during the real mastication of a tough bolus occurred significantly more frequently and with a significantly longer mean duration when compared to the same masticating activity of an age and gender matched asymptomatic control group. Some significant gender differences were also noted within both groups.
Clinical significance
When considering evaluating occlusion for potential interferences it is customary to use a marking medium, instruct the patient to bite into the medium and slide into lateral excursions to mark the teeth. This can identify potential posterior working and non-working interfering contacts. The difficult decision then is to decide which mark or marks need to be adjusted. However, if the patient produces few or no SP while chewing, it means that the interferences present are avoidable. If, on the other hand, the patient produces frequent SP during chewing, the interferences are unavoidable and the patient can most likely benefit from their removal.25
Conflict of Interest
John Radke is the Chairman of the board of directors for BioResearch Associates, Inc. and Parvathi Kadamati is a biomedical engineer.
Funding Statement
No funding or in-kind inducement was received by any of the authors.

._because_there_were_.jpg)





._because_there_were_.jpg)




