INTRODUCTION
Temporomandibular Joint disorders (TMJD) are common conditions that according to some studies, affect up to 28% of the population, although many studies have not included imaging.1,2 Internal Disc Derangement (IDD) is the most frequent cause of TMJD and is defined as an abnormal relationship of the disk to the condyle. This is a structural mal-relationship of all of the components of the TMJ, affecting not only the disc, but also the ligaments, the synovial tissue, the condyle and all of the muscles attached to the mandible. The most common signs and symptoms of TMJD include; a.) pain over one or both of the TM Joints, b.) pain or fatigue while chewing, c.) TMJ clicking or noises, d.) limitation in mouth opening, e.) headache, f.) facial pains, g.) locking of the TMJ, h.) a progressive change in the bite, i.) deviation or deflection while opening or closing and j.) obvious facial asymmetry. The mechanical symptoms tend to be related to the joint, while the painful symptoms are multifactorial.
A majority of the diagnostic tests for TMJD involve indirect testing or clinical examination that often give the examiner a clinical impression regarding symptoms and signs of ligament, disc and/or bony injury.3 The findings of these tests may be consistent with TMJ damage, but may or may not always be definitive and are very dependent upon the diagnostic skill of the examiner. Therefore, positive findings of concern from indirect testing should be followed by further diagnostic tests that could include Orthopantomogram (OPG), Cone beam computed tomography (CBCT) and/or Magnetic Resonance Imaging (MRI), particularly when there are signs and symptoms of structural instability.4–6 OPG is mostly used as a screening radiograph, but the others are used to evaluate primarily bony (CBCT) or including soft tissue abnormalities (MRI). An intermediate clinical step, Joint Vibration Analysis (JVA), is also available to enhance limited clinical diagnostic efficacy and assist the selection of appropriate follow up imaging.
TMJ imaging, although highly dependent upon accurate interpretation, is considered by most as the “gold standard” for the evaluation of the condition of TMJ structures.4 It is mainly indicated when a physical examination suggests a structurally altered TM joint foundation that has signs and/or symptoms of instability. Since JVA is a dynamic test, it also contributes substantially to evaluating the stability of the TMJ. From an imaging perspective, a structurally normal and intact TM joint foundation is based upon seven-disc parameters, three condylar parameters and two skull base parameters.5
The maxillofacial radiologist may detect early imaging indications of degeneration and by initiating treatment, potentially avoid the progression of this condition to its advanced and irreversible stage, which is characterized by severe degenerative changes. Because the clinical diagnostic criteria do not accurately identify correctly the internal derangement diagnoses with the sensitivity and specificity that MRI and CT based images reveal,6 clinicians have often been misled by clinical findings and are therefore unable to effectively rely on them in practice.
OBJECTIVE
The present study aimed to elucidate the interpreted OPG, CBCT and MRI indications of various degrees of TMJD and to correlate them with the clinical signs and symptoms of the Temporomandibular Disorders that are specific to the TMJ.
MATERIAL & METHODS
This study included 31 patients (62 TMJs), who reported to the Department of Oral Medicine and Radiology, Shri Dharmasthala Manjunatheshwara College of Dental Sciences and Hospital (SDMCDS), Dharwad, Karnataka, India with the complaint of TMJD from May 2019 to October 2019. OPG, CBCT and MRI were obtained for both of the TMJs of each patient within a week of the clinical examination. All OPG scans were made with Carestream (Kodak) 9000 machine with exposure parameters of 70 Kvp, 10mA, 15.8s. CBCT scans were made with Carestream(kodak) 9000 machine with exposure parameters of 90 Kvp, 12 mA, 10.8 seconds, with a field of view of 3 x 5 cm for both TMJs. Patients were positioned within the scanner standing straight and were instructed to hold still with their teeth together in maximum intercuspation. The patients were then encouraged to undergo T-1 and T-2 MRI scans of their TMJs in the open and closed mouth positions with a General Electric (GE) MRI machine of 1.5 Tesla and using dual surface coils designed specifically for the TM Joints.
The inclusion criteria were these clinical signs and/or symptoms: TMJ pain, clicking, limited mouth opening, deviation and/or deflection, facial pain, headache, open or closed lock, chewing fatigue, progressive change in the bite and obvious facial asymmetry. All patients with any developmental deformity of the face and/or jaw, with a history of Previous TMJ treatment and/or a history of craniofacial trauma were excluded from the study. All patients provided informed consent and the protocol followed with the World Medical Association’s Declaration of Helsinki.
The signs and symptoms of the patients were tested for correlation with the interpretations of the OPG, CBCT and MRI images. See Figures 1, 2, 3 and 4. Two Oral Radiologists blinded to the clinical signs and symptoms interpreted all the OPG, CBCT and MRI images.
Statistical analysis
Statistical analysis was performed using a commercially available statistical software program (SPSS 19.0, IBM, Armonk, NY, USA). The Fischer’s exact test and the Chi-square test were performed as appropriate for correlation of clinical findings with OPG, CBCT and MRI findings. P < 0.05 was considered statistically significant.
RESULTS
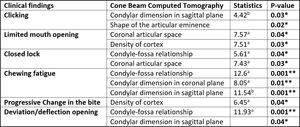
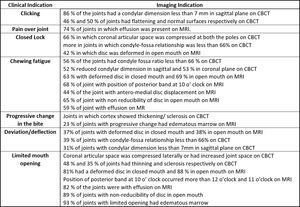
In the study, 25 out of 31 (80%) patients were female patients with the mean age of 29.5 years. Male patients accounted for another 20 percent with the mean age of 20.1 years. None of the clinical findings were significantly associated with OPG interpretations. See Figure 5. and Figure 2. Of the nine TMJD signs and symptoms considered, six of them were significantly associated with CBCT interpretations (p < 0.05), three of them being highly significant (p = 0.001). See Figure 3. Seven of the nine TMJD signs and symptoms were significantly associated with MRI interpretations (p < 0.05) with five of them being highly significant (p < 0.001). See Figure 4. Figure 5 presents the percentages for each of the significant variables.
DISCUSSION
Greater frequency and severity of TMJD in females have been documented in various epidemiological studies.7,8 Although the explanation for the difference has been based on behavioral, psychosocial, hormonal and constitutional factors, no definitive evidence to that effect has been produced or conclusions established.7,9 Most of the patients in this study were females, with male to female ratio of 1:4. This ratio is consistent with previous studies, although some have found an even higher percentage of females.
TMJ clicking corresponds to 26.2% of all clinical signs of TMJD and is the most common complaint of patients.10 Clicking is a major indicator of full or partial disk displacement with reduction (DDWR), folding of the disc when not reducing (DDWOR) and is indicative of abnormal biomechanical forces applied between the disc and the mandibular condyle, which alters their shapes and function.11 Various potential factors are cited in the literature that increase the risk of TMJD; a.) chronic microtrauma or injury to joint during childhood, b.) acute injuries (macro-trauma) directed against the TMJ, c.) shape and/or dynamic property alterations of the TMJ components, d.) a lack of lubrication, e.) modifications of the disc form, f.) degenerative articular disorder, g.) excursive occlusal abnormalities, h.) hyperactivity of the lateral pterygoid muscles, i.) joint hypermobility and j.) weakness or laxity of the TMJ ligaments of the joint capsule.11–13 As shown in Figure 6, clicking was present in 86% of the joints that had a condylar dimension less than 7 mm in sagittal plane on CBCT. See Figures 7 & 8. 46% and 50% of the joints had flattened and abnormal surfaces respectively on CBCT. See Figure 9. Hence our findings are in accordance with the literature.
The clinical findings of pain over the joint was associated with 20/27 (74%) of the joints (See Figure 6) in which effusion was present on MRI, See Figure 10. TMJ effusion typically appears as a bright signal on T2-weighted MR images.14
It has been suggested to indicate fluid representing intra-articular inflammation and is considered by some to be a sign of synovitis.15,16
Although the exact etiology of effusion is unclear, it is mostly found to coexist with non-reducing disc displacement in the joint.16–24 This mal-relation of the disc to the condyle leads to deterioration and abrasion of the articular cartilage and disc surfaces, in turn leading to a release of pro-inflammatory cytokines including TNF-alpha, nitric oxide, bradykinin, IL-6, IL-1, IL-8, and leukotriene B4.24–26
These cytokines create a painful inflammatory effusion around the joint leading to further joint destruction. Some authors have found a significant association between TMJ pain and the increased signal intensity of effusion,27–29 while two limited studies were unable to correlate TMJ effusion to presence of TMJ pain.30,31
Closed lock is most often an indicator of disc displacement without reduction (DDWOR) with limited mouth opening. In the closed-jaw position, the disc is dislocated anterior to the condylar head, and does not reduce with jaw opening. This causes a mechanical obstruction to the normal translation of the condyle. An alternative less frequent cause of limited opening is muscle trismus, but usually only after an overt facial trauma or extraction of 3rd molars. In the present study closed lock was present in 66% of the joints in which coronal articular space was compressed at both of the poles on CBCT (Figure 11.), in joints where the condyle-fossa relationship was less than 66% on CBCT (Figure 8) and 42% of joints in which disc was deformed in open mouth (Figure 12.) on MRI. All these indications in this study were either suggestive of anterior disc displacement without reduction or were consequences of it.
A study was done by Nielsen et al in 1990, which stated that subjects with TMJD pain alter the recruitment of their jaw muscles.32 Free nerve endings act as nociceptors activated by noxious stimulation such as temporo-mandibular joint overloads and/or masticatory muscle ischemia when it is prolonged and associated with muscle contractions.33–35 A decrease of motor unit firing rate has been correlated to the intensity of muscle pain, but the central mechanisms involved remain unclear.36 All the radiographic findings in our study, which were associated with the clinical finding of chewing fatigue, were suggestive of chronic internal disc derangement. See Figures 6, 12 & 13.
Progressive change in the bite indicates an active osteoarthritis, that occurs from abnormally elevated loading of articular surfaces. In the initial stage it is associated with concavity or flattening of articular surfaces, while the marrow signal remains normal. As the condition becomes chronic, the localized deformity along with edema in subarticular marrow can be seen.5 In this study 3 out of 13 joints with marrow edema seen on MRI and those in which cortical thickening and sclerosis were present, were associated with clinical findings of progressive change in bite. See Figure 14. Hence, the findings were in good agreement with the most current literature.5
Deviation is typically a sign of internal disc displacement with reduction, while deflection is commonly associated with disc displacement without reduction. All the radio- graphic findings in Figure 11 were suggestive of internal disc derangement and hence were in agreement with the structural clinical signs and symptoms.
The Figure 6 indications that are significantly associated with limited mouth opening are suggestive chronic disc displacement without reduction, with or without degenerative changes, which prevent normal condylar translation due to mechanical obstruction, due to pain or due to both.
LIMITATIONS
The study sample could have been larger and a more heterogenous population of TMJD patients. In future, imaging data could be correlated with clinical, radiological and biometric data, such as EMG and Jaw Tracking with JVA, which could establish enhanced clinical protocols for effective TMJD diagnosis and enhance the selection of the most appropriate imaging tool.
CONCLUSIONS
The results illustrate the relatively well-established correlations between the structural clinical signs and symptoms of internal derangements with CBCT and MRI imaging of TMJ dysfunctions, but no correlations were found with the purely painful symptoms (e.g. headache, orofacial pain, etc.). However, the precise interpretation of those clinical signs and symptoms is unreliable because it is usually only possible to detect clinically that some type of structural problem exists within the TMJ. To define TMJD conditions precisely, it is usually necessary to utilize advanced imaging technology.
To understand the discrepancies between imaging interpretations and the interpretation of patient symptomatology requires substantial expertise. The differences are best resolved from the direct visualization of joint structures. Whenever there are signs suggestive of TMJ structural instability, clinical examination should be supplemented with CT and/or MRI.
Statement of conflict of interest
The authors declare no conflict of interest.
Funding sources
No commercial or other funding was received.
_clinical_signs_and_symptoms_and_orthopantomogram_interpretations__b)_cone_beam_computed.jpg)











_clinical_signs_and_symptoms_and_orthopantomogram_interpretations__b)_cone_beam_computed.jpg)












