Historical Perspective and Clinical Relevance
Occlusion is the way in which the maxillary and mandibular teeth come together. This definition is describing a static relationship. However, in function the teeth move across one another, and dynamic occlusion is what is then critically important.
Occlusal appliances are often recommended for the symptomatic treatment of temporomandibular disorders (TMD), that appear to result from TMJ internal derangements, particularly from reducing displaced disks.1–7 Occlusal coronoplasty is more often recommended for TMD patients with primarily muscular symptoms.8–11
Historically, the cited goals for occlusal splints are to eliminate occlusal interferences, create stabile TM joint relationships, and limit the damage caused by parafunctional habits. Splints have also been used diagnostically, as an indirect method of altering the occlusion.2–7
The Occlusal Disengagement theory proposes that the use of a properly adjusted appliance can reestablish proper occlusal relationships. The rationale of splint implement is to eliminate the negative occlusal contact stimuli that cause muscular hypertrophy during mandibular function, while providing proper TM joint support. Alternatively, the Maxillo-mandibular Alignment theory proposes that when the mandible is mal-positioned relative to maximum tooth intercuspation, occlusally-generated symptoms can arise within the Stomatognathic System, that often can (theoretically) be eliminated when the mandible is repositioned. Splints can therefore be an intermediary step in the treatment process, by adapting the splint’s occlusion to an achievable, and more orthopedically stable, TM joint position.
Mastication itself, is the most important function of the Stomatognathic system. Gibbs and Lundeen used the Gnathic Replicator to demonstrate that some occlusal contact occurs during chewing, which can influence both the opening and closing pathways.12 Then Wood using a Kinesiograph, confirmed that cuspal forms can cause changes in the mandibular chewing movements, once the food bolus has been masticated to a homogenous consistency.13 It is clear that Occlusion plays a critical role in mastication. But to date, only Disclusion Time Reduction (DTR) therapy with the Immediate Complete Anterior Guidance Development coronoplasty (ICAGD),14 which alters the occlusion with very specific, time-based excursive movement occlusal corrections, has been shown to functionally improve human mastication.15 Given these observations, it follows that the topography of teeth and dental restorations can cause changes in mandibular movement patterns.
The clinically relevant questions are, when should occlusal relationships on a splint or a natural occlusion be evaluated? And are patients cognizant of these occlusal discrepancies? Regardless of one’s occlusal philosophy, the operator must evaluate the force and time components of a patient’s occlusion, before any proper and measured refinements of the occlusion should be made.
Spear has noted that the one thing virtually all occlusal philosophies agree on in today’s occlusal thinking, is that quality occlusion would demonstrate even, simultaneous intercuspated tooth contacts on all posterior teeth, and that the canines should also occlude in centric closure.16 The literature is clear that an ideal occlusion should include the following criteria17:
-
Occlusal forces are applied to the long axes of the teeth.
-
In lateral excursion, teeth immediately separate in the non-working and working posterior dentition.
-
Anterior teeth disclude the posterior teeth in protrusive and lateral movements.
-
Posterior teeth contact more heavily than anterior teeth in centric occlusion.
Dentistry has used these principles to guide clinicians when restoring teeth prosthetically, or when treating TMD symptoms with splint therapy. Consequently, not adhering to these ideal principles can result in damage to the osseous support of both teeth and dental implants.18,19 A clinical concern then becomes when is the best time to evaluate and revise occlusal contacts? A review of the literature suggests that the time of day when a patient’s bite is registered, may be a factor that significantly affects their bite status.20,21 Therefore, the Specific Aim of this pilot study was to utilize the T-Scan technology to measure and compare the first tooth contacts in 32 patients, who were recorded at 2 distinct time-points in the same day, while the subjects self-guided into Maximum Intercuspation (MIP).
METHODS
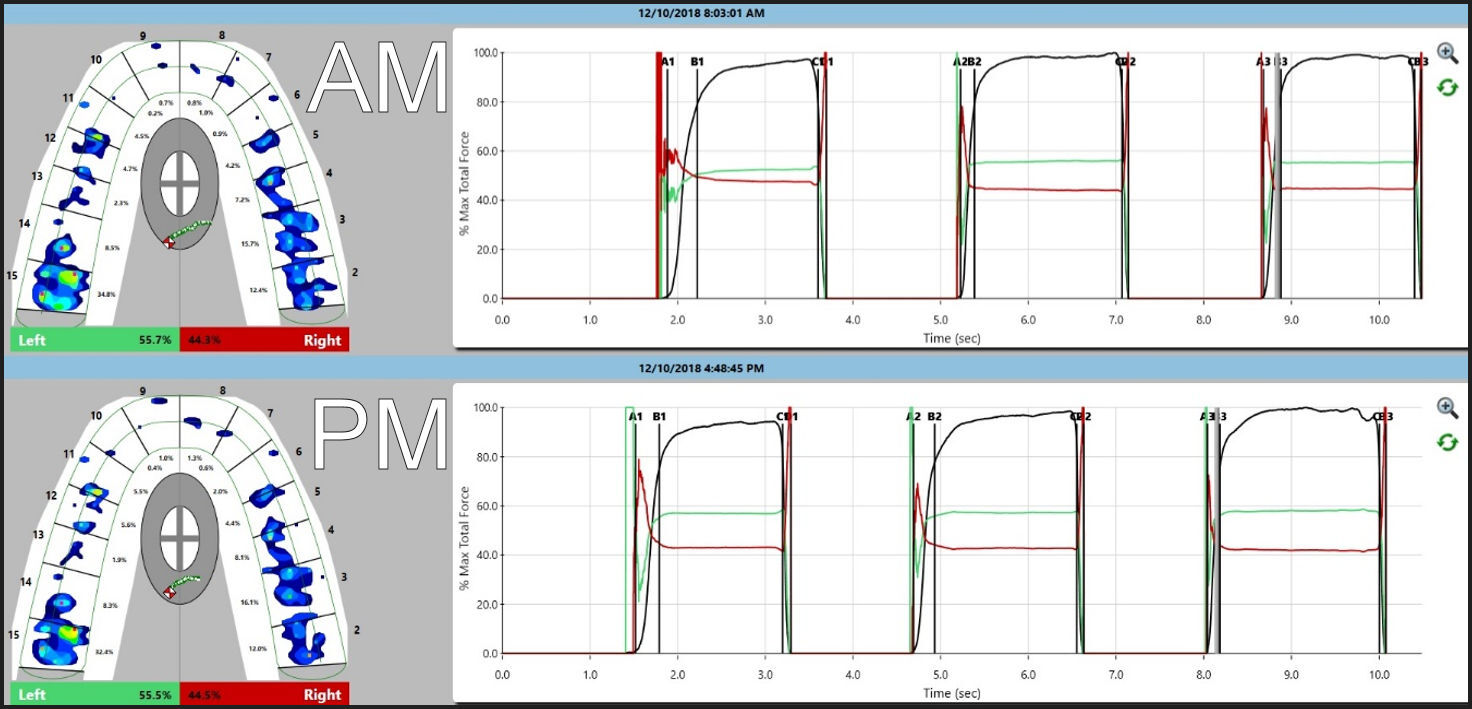
Thirty-two (32) volunteer asymptomatic subjects had their occlusion times and opening disclusion times recorded with the T-Scan (T-Scan 10, Tekscan, Inc. S. Boston, MA, USA). All subjects were fully informed that no treatment was to be provided, and they consented to the testing of their occlusions. All subjects had Angle’s Class 1 occlusion. Every subject conditioned a new Novus HD sensor (Tekscan, Inc. S. Boston, MA, USA) with three intercuspated crushes prior to any measurements being made, with the recording sensitivity adjusted appropriately to ensure only 3 pink sensel were obtained at maximum bite force. Two important software settings were adjusted prior to any recordings being obtained. First, Turbo Mode was turned on. This feature allows the software to record more frames per second, in increments of 3/1000th of a second. And “Triggered Scan Start” was turned off, as this feature starts recording automatically when teeth start to crush the sensor. Since we were evaluating first tooth contact, Triggering was turned off to avoid the elimination of any early occlusal contact data possibly present at the beginning of the recording. Subjects sat upright in a dental chair for the recordings. Then participants self-closed into their MIP crushing the sensor three times, to record their occlusal force profiles, and their occlusion times and the opening disclusion times. This protocol was conducted first at 8 AM and then at 5 PM on the same day, to detect differences in the first tooth contact at two different times of day. After all of the participants had completed the protocol, the T-Scan data was statistically analyzed.
T-Scan recordings were reviewed manually in playback mode to review the first tooth contact of significance in each of the 3 patient self-closures. Mean and standard deviations were calculated for each subject’s occlusion times and each opening disclusion times (Tables 1 and 2). The AM and PM means were then tested using the Mann-Whitney signed-rank test. The Null hypothesis was that there would be no difference between the AM and the PM 1st tooth contacts. Alpha was chosen at p < 0.05.
RESULTS
In the 3-bite sequence no significant change was found in the mean occlusion time of the first bite, but the second and third bites were significantly slower at PM than at AM (p < 0.05) (Table 1).
Comparing the first 2 mean opening disclusion times, no significant differences were found. But the third mean opening disclusion time was significantly shorter in the PM than in the AM (p = 0.0414) (Table 2).
Change in first contact location
Of the 32 patients recorded, 26 (81%) showed no change in the first tooth contact location (Figure 1). However, the remaining 6 (19%) did show a change (Figure 2).
The force profiles (the distribution of force around the arch) varied between 3-5% when comparing intra- and inter-arch scans. This is a known and acceptable variation seen repeatedly among symptomatic and asymptomatic patients.12 Overall, the Center of Force trajectory patterns did not change from AM to PM. Also noteworthy was that the bite force profiles and the bite timing data did not noticeably change, staying ≤ 5%.
It is important to report that none of the patients could perceive bite force or timing variations. This is an interesting finding because dentists often make assumptions like, “if the bite is off, the patient will be able to tell me.” Dentists rely on patient “feel” feedback as part of co-diagnosing chief complaints involving tooth pain or sensitivity. But the patient’s perception of their occlusion does not always manifest in a repetitive manner.
It is also important to state that most of our restorative dentistry is conforming in nature, meaning it must work within the existing occlusal relationships to be accepted by the patient. What happens when a new restoration is not designed to work within the existing occlusion, and instead actually changes it?
Incidental Findings
While compiling data, an interesting observation was made in that 56% (N=18) of the participants had 30% or more of their total bite force concentrated on one tooth. And importantly, that overloaded single tooth was restored with either an onlay or a crown. Figure 3 is a representative example of this observation.
DISCUSSION
Shafagh et al., studied 13 Angles Class 1 occlusion subjects with and without obvious ‘physiologic dysfunction’ by comparing their CR mountings at various times of day.21 The authors were searching for circadian rhythm changes in CR throughout the day. Their results indicated that:
-
Sequential centric relation positions were repeatable for a few subjects, but most demonstrated variability in their CR registrations
-
In many subjects, the morning CR position had a more anterior-inferior position of the condyles, while the night CR position was the most posterior-superior position of the condyles.
-
The evening seemed to be a better time for making CR records, if the most posterior-superior position of the condyles was desired.
-
This study supported the theory that some freedom in the centric position should be incorporated into the occlusal scheme.
This 1st tooth contact study evaluated 32 subjects by comparing their MIP force profiles using T-Scan 10 at two different time points in the day, to detect possible changes in the first tooth contact. The findings were:
-
81% of the subjects showed no change in their first tooth contact, while 19% did show variations in their first tooth contact.
-
Subject force profiles did not change in any subject, regardless of whether their initial tooth contact changed or remained consistent.
-
The Occlusion Time into MIP, and the and Opening Disclusion Time out of MIP did not change from AM to PM.
-
This study’s observations were somewhat consistent with Shafagh’s findings, in that some degree of freedom in the TM joints would likely result in slight variations in how the teeth come together in MIP.20 Also important to consider is that the articular disc is 80% compressible,22 whereas teeth represent a hard stop and compress comparatively very little when the PDL is engaged.
Limitations
One limitation of the study was no effort was made to separate asymptomatic from symptomatic TMD patients. Another limitation was that only 32 patients were recorded yielding a low number of participants. However, after recording 20 total data sets, the statistical results changed very little (less than 3% overall), such that a decision was made to cease recording any new data
Conclusions
Statistically significant but very small differences were found for this group of 32 subjects between the AM and PM mean occlusion times and mean opening disclusion times. Although it is questionable whether such small differences are clinically relevant, a very high level of consistency was obtained within all the recorded measurements. Additional research may help determine whether a 30 - 50 millisecond increase in the occlusion time, or a 56 - 69 millisecond reduction in the opening disclusion time, has some clinical impact on a patient’s occlusal health.