INTRODUCTION
Temporomandibular Disorders (TMD) represent an ensemble of clinical presentations with signs and symptoms related to impaired function of the stomatognathic system.1 The symptoms vary but may express themselves as pain or tenderness of TMJs area, clicking or grating sounds in the TMJs, limited jaw movements, muscle pain, headache, tinnitus, impaired hearing, earaches, and others. The etiology is multifactorial and can include occlusal, muscular, articular, cervical, stress and general health factors. The diagnosis and treatment of TMD warrants a multidisciplinary and interdisciplinary therapeutic approach focusing on TMJs and all the associated structures and systems including the neuromuscular system.2
The prevalence of TMD varies depending on the studies, the diagnostic criteria and populations evaluated. In a study examining the Research Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD) Axis II, 36.2% of the population had some degree of TMD pain.3 Data from another study reported that the prevalence of one or more symptoms of TMD was 27.7%, while the prevalence of one or more signs of TMD was 64.4% which were mild in severity.4 Looking at an intra-articular sub-type of TMD, it was found that the overall prevalence of clinical signs was 16%.5 The prevalence for the muscle disorders sub-type of TMD was 88.7%, while the presence of disco-pathosis or arthropathies ranged from 26.3% to 42.8%.6
A review of the literature, from 2012, found a lack of evidence of a link between occlusion and posture, and that the presence of TMD was not related to any occluso- postural abnormalities. The authors of this review went further and suggested erroneously that instrumentations that measure occlusal, electromyographic, kinesiographic or posturographic parameters should not be used in the evidence based TMD practice and stated, “they appear to be a clinical non-sense”. Contradicting their concern they continue, “The adoption of instrumental devices to assess dental occlusion and body posture has to be reserved to strictly controlled research settings, with the aim to clarify the main doubts concerning the high inter-individual variability of the occlusion–body posture–TMD relationship.”7
Other clinicians continue to measure, observe, and publish correlations between occlusion and posture through clinical cases, studies and objective data from biometric measuring instrumentations.8–10
Human bipedal upright stance is intrinsically unstable and is achieved through a complex neurological sensory feedback process involving the integration of sensory information from multiple sources, visual, vestibular, and somatosensory. This information is continually re-evaluated to maintain a body erect.11,12
Posture itself is an extraordinarily complex and dynamic accommodation process, represented by various biomechanical models.13 The postural tasks and controls can be appropriately evaluated in any population of study subjects using technological tools and tests.14 The reliability and validity of center of pressure (COP) based parameters have been found in older adults15 as well as children and adolescents.16 The Mat-Scan® has been validated to measure the COP.17
It was demonstrated that the individual-specific sway indices correlated more significantly with body parameters than the universal indices. This suggested that individuals’ biomechanics are characterized by the individuals’ features of postural sway rather than neural control.18
A study has shown that posture and occlusion have a reciprocal relationship, where changes in occlusion generate changes in posture and changes in posture generate changes in occlusion.19 Research continues to accumulate confirming the relationship between occlusion and posture and postural balance.20–23
“Robust sway reduction during feedback-controlled biting tasks in healthy subjects involved a stiffening phenomenon that was attributed to the common physiological repertoire of posture control and might optimize the stability of posture under these conditions.”24 Modification of the occlusion using stabilization splints modifies the peripheral information received by the central nervous system, leading to changes in the corporal postural tone.25 In an epidemiological study of 605 primary school age children were examined. Postural, orthoptic and occlusal factors were found to be clinically related.26 In respect to the actual medical principles, viewing the human body in a holistic manner, this study presented an interdisciplinary correlation to the incidence of dental malocclusions together with posture and eye convergence disorders.26 Similarly, another study compared the postural stability of individuals with and without signs of TMD using a stabilographic platform. The results showed a significant difference in sway parameters, cervical pain, postural asymmetry, and postural instability in individuals with TMD.27
Malocclusion and postural body stability have an inverse relationship, the worse the malocclusion, the less stable the posture.28 It was observed that a whiplash induced instability of posture contributes to an increase in muscle tone, teeth clenching and symptomatology of TMD in subjects with malocclusion.29 Patients with temporo-mandibular disorders have demonstrated disruptive influences on body alignment, increased level of pain symptoms and poor postural stability.30
Interestingly, the interdigitation of the teeth affects neuromuscular co-contraction patterns, resulting in increased kinematic precision of standing.31 These results and others suggest that the postural stabilization of the jaw comes from a functional coupling of the craniomandibular and postural systems.32
It has been demonstrated that cranio-cervical functional parameters differ in TMD patients compared to healthy individuals. There is alteration in the occipito-atlanto space, there is a decrease in the craniovertebral angle, there are alterations in the hyoid triangle, in the depth of the cervical spine and in the morphometry of the cervical vertebra.33 Based on these results, these authors concluded that there is a different relationship between the anatomical and functional parameters of the cervical spine in patients with TMD compared to healthy patients.34
The head and neck can be looked upon as an inverted pendulum, stabilized by neuromuscular forces. The dynamics and the mechanics of the lower jaw and the temporomandibular joint couple into the pendulum’s stabilization process. Alterations or pathologies of the TMJ lead to perturbation of the forces acting on the head and neck which leads to symptoms and degeneration.33
An inverted pendulum dynamic model analyzed the biomechanics of traumatic neck injuries suggesting the possible roles of the stomatognathic system, mandibular dysfunctions and dental malocclusion, within the cervical spine disorders.35
It has been demonstrated that an occlusal splint can have a direct influence on the cranio-cervical relationship. A comparative study of cephalometric analysis, before and after the insertion of the oral appliance, revealed a significant head extension over the cervical spine, accompanied by a decreased lordosis, notably at the first three cervical vertebrae. It was suggested that these changes reflect a compensation mechanism.35
This paper presents a retrospective cohort study of existing data from clinical cases of TMD patients that were treated with an adjusted oral orthotic, a change in dental occlusion, and their immediate response in postural parameters recorded on the Mat-Scan® force platform by Tekscan (Boston, MA USA).
METHODS & MATERIALS
Patient Selection
Clinical case subjects were selected from a clinical private practice (Dental Health Centre, Dieppe, New Brunswick, Canada). The data from the last 25 consecutive new patients were selected for the evaluation. However, 2 patients were eliminated when some data were missing. All were women between the ages of 18 and 66. All presented signs and symptoms of TMD at their examination, in accordance with the Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications.36 The average age was calculated at 49 years old.
Orthotic
The oral appliance (Figure 1) was fabricated on articulator mounted stones models, from alginate impressions of the patient’s dentition. The Fox plane37 was recorded and used as the occlusal plane when mounting the maxillary model on a Corident (Daegu, Korea) semi-adjustable articulator. The lower model was mounted using a phonetic bite.38 A thermoforming material from Erkodent (Pfalzgrafenweiler, Germany), Erkodur,® 1.0 mm, was formed to fit the mandibular model before an orthodontic resin from Dentsply (Milford, USA) was applied to fabricate the orthotic. Bilateral contacts were established on the articulator and adjusted with occlusal paper, Bausch (Koln, Germany) PROGRESS 100® articulating paper 100 microns. Upon delivery of the orthotic, contacts were adjusted with digital occlusal scanner T-Scan®, version 9, from Tekscan (Boston, USA) to obtain symmetry of the contact forces and timing.39,40 See Figures 2a and 2b.
Postural Sway Recording
The methodology for sway recording has been described elsewhere.41 Briefly each recording is performed with eyes closed and teeth together for 30 seconds on Mat-Scan®, Footmat Research version 7.10 (Tekscan, South Boston, USA) using a foot template to ensure consistent foot position across all subjects and eliminate a potential confounder.
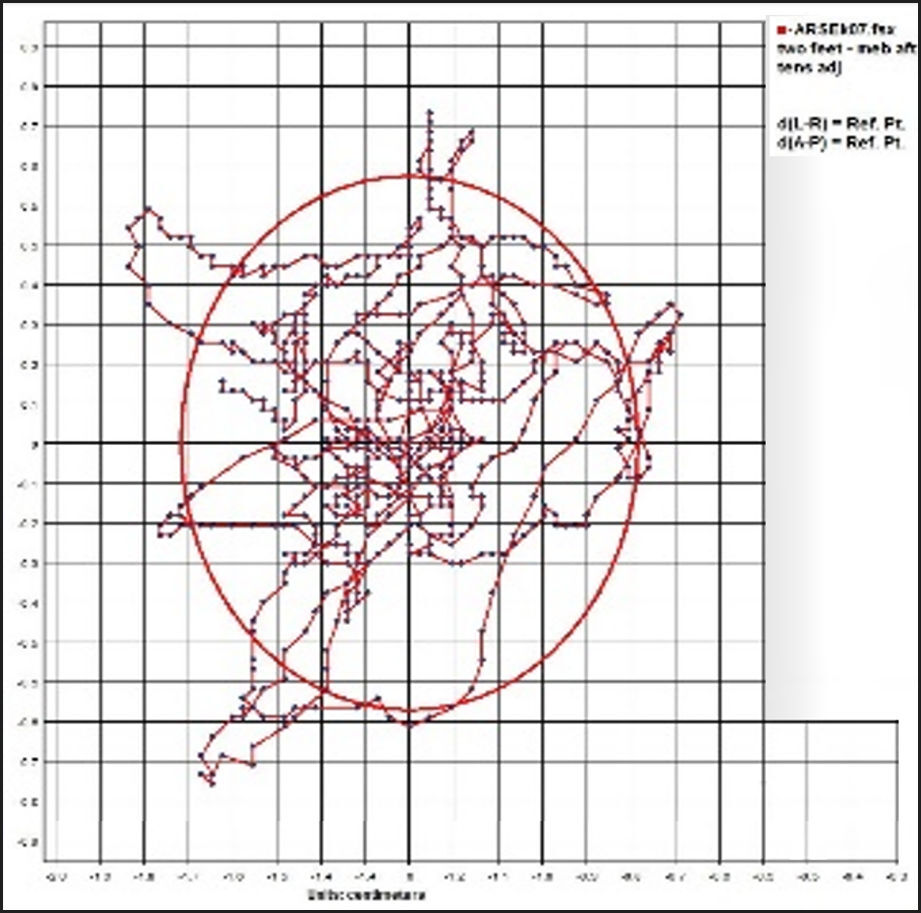
The recordings were conducted within a single appointment on the day of delivery of the orthotic and corresponds to the immediate postural response of the body. The initial recording of the habitual bite was done at the beginning of the appointment (See the example in Figure 3) and the second recording with the oral orthotic in place was done at the end of the same appointment (See the example in Figure 4), then comparisons made between the scans (See the example in Figure 5).
Cephalometry
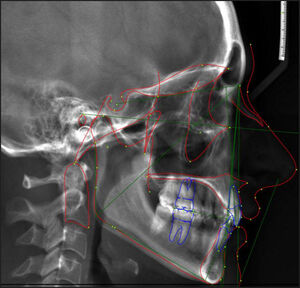
Each subject underwent a radiographic cephalometric evaluation with and without the mandibular orthotic to document the change in jaw position and occlusion.
The images were taken teeth in contact with the opposing teeth or against the oral appliance using digital tracing and computing using Dolphin® software (Verona, Italy) by an experience technician/operator at Orthodent Dental Laboratory, Oshawa, ON, Canada See Figures 6a & 6b.
Statistics
All statistical analyses were performed using SAS, Version 9.3 (SAS Institute, Cary, North Carolina, USA). Because of the relatively small sample size (n = 23) and the paired nature of the data (with and without oral orthotic, and open/closed), the Wilcoxon Signed-Rank Test was used to compare changes in linear, angular, and cephalometric measurements. All values of p < 0.05 were considered statistically significant.42
Ethics and Consent
This investigation corresponds to a retrospective study of already existing clinical data, not experimental research. It was determined that ethical approval and consent was unnecessary for the re-collective examination of already existing data from a clinical data base. No personal, medical or other sensitive information was included in the study.
RESULTS
Sway Parameters
The parameters recorded on the Mat-Scan force platform consisted of the area (cm2), the distance (cm), the antero-posterior excursion (cm) and the right-left excursion (cm).
The results are tabulated in Figure 7, under the heading of Sway Parameters. All parameters showed a statically significant difference between the habitual occlusion and the orthotic position (p < 0.0001). There were significant reductions in all sway parameters tested under the orthotic condition, providing a clear indication of the postural stabilization of the TMD patients with this treatment modality. It is known that a reduction in sway parameters corresponds to the stabilization of the body.12
The antero-posterior excursion is the front and back sway measured in cm. It reflects the overall decline of the posture control function. The increase sway in the AP direction relates to a decline in the muscles involved in maintaining the upright posture.43 The reduction in the AP sway brought by the oral orthotic compared to the habitual occlusion (from 3.13 cm to 2.14 cm) was significant (p < 0.0001).
The left-right excursion is the side-to-side sway measured in centimeters. It seems to reflect the labyrinthine righting reflex function of the upright posture. During fatigue, nerve function declines and sway increases.44 Once again, the reduction in left to right sway, induced by the oral orthotic compared to the habitual occlusion (from 1.75 cm to 1.17 cm) was significant (p < 0.0001).
The area measured in cm2 corresponds to the displacement of the center of pressure (COP) in the two dimensions (A/P and L/R) during the recording time of 30 seconds. The larger the area, the more displacement of the COP and the less stable the posture.
The reduction in sway area with the oral orthotic compared to the habitual occlusion condition (from 2.50 cm2 to 1.28 cm2) was significant (p < 0.0001). The results are presented in Figure 8 clearly demonstrate a reduction in sway area with the interposition of the oral orthotic.
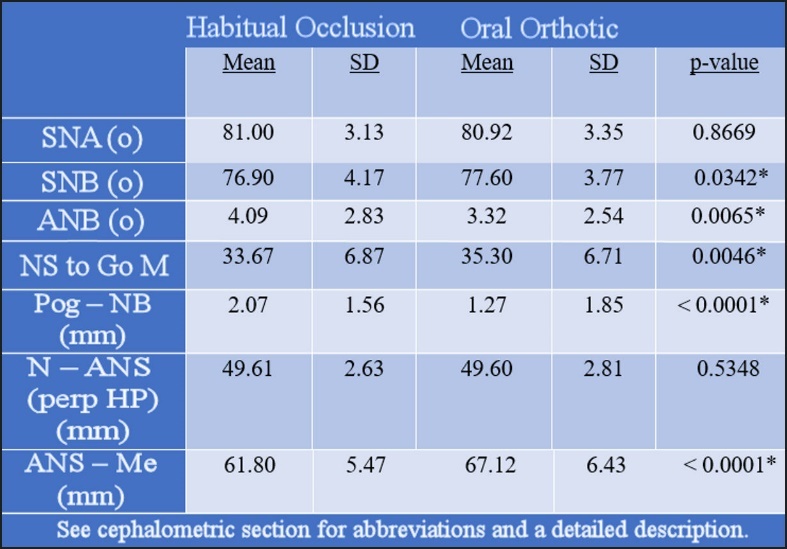
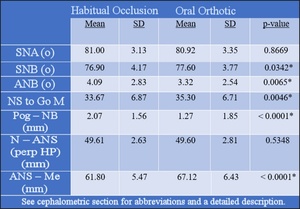
Cephalometric Analysis
The results of the cephalometric analysis are tabulated in Figure 9. The Cephalometric points correspond to the anatomical hard tissue points are shown in Figure 10 for reference of the points used in calculations.
Sella (S) is located in the center of the Sella turcica, Nasion (N) is located in the most inferior, anterior point on the frontal bone adjacent to the frontonasal suture, Point A (A) is located at the most posterior part of the anterior border of the maxilla, near the apex of the central incisor root, Point B (B) is located at the most posterior point on the shadow of the anterior border of the mandible, near the apex of the central incisor root, Anterior nasal spine (ANS) is located at the tip of the bony anterior nasal spine at the inferior margin of the piriform aperture in the midsagittal plane, Pogonion (Pog) is located at the most anterior point of the chin, Menton (Me) is located at the most inferior point of the chin, Gonion (Go) is located at the midpoint of the angle of the mandible where the mandibular and ramus planes bisect.
NS corresponds to the cranial base reference line drawn between Sella and Nasion (S- N)
SNA angle relates the antero-posterior position of the maxilla. The lack of changes between the two conditions of this study indicates that the maxilla did not change position, it remained stable and unchanged in reference to the cranial base.
SNB angle relates the antero-posterior position of the mandible. The significant changes (p = 0.0342) indicate an actual change in the mandibular position in reference to the cranial base.
ANB angle relates the antero-posterior position of the maxilla to the antero-posterior position of the mandible. The significant changes (p = 0.0065) indicate an actual change in the mandibular position in reference to the maxilla.
Go-Me represents the mandibular plane from a line drawn between menton and gonion (Go-Me).
NS to Go-Me represents the angle from between the cranial and mandibular reference planes and indicate and change in vertical dimension of occlusion. The significant change (p = 0.0046) indicates that a change of the vertical dimension of occlusion occurred with the insertion of the orthotic compared to habitual bite.
Pog - NB represents prominence (antero-posterior position) of the bony chin (Pog point) in reference to the Nasion Point B line the Reference Line: Nasion - B point
The prominence of the bony chin (not to be confused with the soft tissue chin) is measured by the distance from the Pogonion to the NB line. This value is affected by the rotation of the mandible; an anterior-superior rotation increases it, while and inferior-posterior decreases it. The significant decrease (p < 0.0001) indicates an inferior-posterior repositioning of Pog relative to the NB line, thus and increase in vertical dimension of occlusion.
N-ANS is a Linear measurement determined by the junction of the N and ANS corresponding to the superior anterior height of the face. The absence of change indicates a constant position of the maxilla and cranium.
ANS-Me is a vertical measure in millimeters determined by the junction of Me and ANS and corresponds to the inferior anterior face height. The significant changes (p < 0.0001) clearly indicate a change in vertical dimension of occlusion with the interposition of the oral orthotic.
The statistical analysis of the changes in the mandibular jaw position from the oral orthotics was significant. This indicates that the oral appliance truly offers a new jaw position and therefore changes the occlusal relationship of the maxilla to mandible in TMD patients.
DISCUSSION
The data presented in this retrospective study of existing patients provide objective measurement and evidence of the postural stabilization following changes in dental occlusion, via the interposition of an oral orthotic between the teeth of maxillary and mandibular arches. The cephalometric analysis demonstrates a significant change of mandibular position in relationship to the maxilla and cranial base. The unchanged position of the maxilla and the cranial base confirm the change in mandibular position only which corresponds to an undeniable change in occlusion. The postural sway measures represent the immediate changes in postural sway recorded on the same day of delivery of the orthotic; it was previously demonstrated that the COP displacements were well reproducible within-day, but had significant between-days variations; therefore, COP assessments should be performed in the same session.44 Each patient acts as its own control in this intra-subject comparation, the difference being only the change in occlusion provided by the oral orthotic. It was noted that body sway during quiet demonstrates subject-dependent variability, making inter-subject comparison difficult.18 It should be emphasized that inter-subject comparison of postural sway may not be achievable due to these important individual variabilities when it comes to postural sway.
This retrospective study of clinical case results supports a previous study that demonstrated a stabilization of posture in the stomatognathic system with the interposition of an oral appliance between the maxillary and mandibular jaw. The deficit in balance, which correlates with increased body sway, was improved with a change in the bite position.45 Similarly, in athletes, the insertion of an anatomic sports-guard provided postural stabilization compared to habitual bite or a flat plane sports guard which did not.41,46 This is in contrast with others who did not find a correlation between dental occlusion and body posture.47
Occlusal splint therapy is one of the most-studied treatment modalities for the treatment of TMDs, providing pain relief or reduction in the most acute or chronic TMD patients.48 Occlusal appliance therapy provided pain reduction, movement symmetry of the condyles, relaxation of the jaw muscles and increased activity during maximum intercuspation. One study found functional Magnetic Resonance Imaging (fMRI) showed a decrease activity in the right anterior insula and right cerebellum with a properly functioning stomatognathic system. “Correlation analysis between pain score and fMRI activation decreases identified right anterior insula, left posterior insula and left cerebellar hemisphere. Left cerebellar and right primary motor activation magnitude was negatively associated with symmetry of the condylar movements.” The anterior insula impacts the monitoring of TMJ pain. Also, the improvement in the symmetry of movement of the condyles was associated with a decrease of activation in primary motor and cerebellar cortex.49 It is therefore accepted that the therapeutic benefits of an oral appliance go beyond a physical crutch and act at the neurological level via both peripheral and central nervous system. These details should be further studied.
The concept of TMJs adapting to occlusion or malocclusion is supported by a recent publication. The development of malocclusion or the mal-adaptation of the stomatognathic system seems responsible for the development of TMD.50 In animal models, the creating of malocclusion or non-matching cusp-to-fossa occlusal relation leads to degenerative changes of the condylar cartilage.51 It provides an answer to which came first; it seems that malocclusion is responsible for the deterioration of the TMJs.
TMD is considered to have a multi-factorial etiology. Genetic, physiologic, traumatic, pathologic, environmental, and stress are factors. “Nonworking side contacts, slides between retrusive-intercuspal position (RP-IP), increased vertical or horizontal overlap and loss of occlusal stability due to missing posterior teeth are all occlusal factors related to signs and symptoms of TMD.”52 Some speculate that individuals may adapt to occlusal discrepancies with the absence of signs and symptoms of TMD, but it is impossible to predict who will adapt or not. The integrity of the stomatognathic system must be evaluated at rest and in function prior to occlusal treatment to “determine the occlusal modification necessary to achieve a simultaneous contact of the maxillary and mandibular teeth while the articular elements are in apposition.”52 This was achieved in the current study with the fabrication and adjustment of the oral orthotic with T-Scan®.53
The positive effects of a mandibular advancement appliance (MMA), in the improvement of the cervical lordosis, has been demonstrated in TMD patients with chronic cervical pain. The researchers concluded that the craniocervical relation should be evaluated initially and after the delivery of the appliance.54 The present study went further and evaluated the postural stabilization of the whole body. The results reported here agree with another study that found the skeletal malocclusion class and the interposition of occlusal splints affect the cephalometric analysis measurements, which correlate with a change in postural sway in stabilometric recording.55
The stability of a standing body has been postulated to result from five postural chains, emerging from the head. There are three antero-posterior chains: lingual, facial and central, responsible for the equilibrium antero-posterior and where the mandible is the regulator. There are two other lateral chains called masticatory: antero-lateral and posterolateral. The posture reflects the structural integrity of these chains.56–58 The assessment of global body posture misalignment revealed that TMD subjects had more pronounced postural changes compared to healthy subjects. All symptomatic subjects presented abnormal distributions of the plantar pressure, indicating that TMD influences the postural system.59
It can be suggested that in the presence of TMD, there is a disturbance of the postural chains, leading to instability of posture that can be corrected with the interposition of an adjusted oral orthotic. Others have found that TMD subjects showed a morphological and functional alteration of the cervical spine, shoulder posture and postural deviations of the antero-internal hip chain.60
The physiological chains61 may provide an explanation of this complex relationship and deserve to be considered in a multidisciplinary and collaborative approach to patient care. The integration of biometrics and digital technologies should become part of the daily dental medicine practices to objectively measure, document and provide data to the clinicians in the diagnostic examination, treatment planning and outcome monitoring.62,63 The clinicians and health professionals must also adopt a more holistic view to the individual patient and consider a global approach to treatments. The teeth should no longer be considered independent appendages solely responsible for chewing, but integral entities part of a very complex ensemble of systems interdependent on each other in an organism.64 Biometrics provide parameters unknown otherwise, that are changing the view the stomatognathic system, including the parameters that define occlusion.65
Limitations
This retrospective study presents robust data with some significant differences, but it also has some limitations. The size sample was limited to 23 subjects. A larger cohort should be considered to repeat the study and confirm the results on a larger scale. Because subjects were selected as consecutive patients presenting to a dental clinic and the random nature that entails, they were not matched by sex and age. In fact, all study subjects in the cohort were TMD patients of the female sex. The study was also an intra-subject comparison, where each one acts as their own control. Some may suggest that having a second group as controls, but this may or may not be advisable based upon the fact that body sway during quiet demonstrates subject-dependent variability. The study should be repeated in the future and address some of these limitations at a larger scale.
CONCLUSIONS
The analysis of the presented clinical data provided significant and objective evidence of the postural stabilization of the body through changes in dental occlusion and mandibular jaw repositioning with an oral orthotic. The results confirm the existing relationship between the stomatognathic system and the body posture. Although the exact mechanisms of this interaction remain to be fully elucidated, it certainly exists. It is imperative that treatment of temporomandibular disorders include the concepts of occlusion, together with the objectivity of biometric measurements. Relying solely on subjectivity and opinions should be relegated to the past. It is not in the best interest of the profession or the patients to ignore biometric technologies. Changes in occlusion produce a phenomenon of Bio-Functional Neuro-Reprogramming within both the stomatognathic system and within the whole body. It is recommended that further work be done in this area with a larger and more homogeneous sample.
Conflict of Interest
There is no source of any conflict of interest from any of the authors.
Funding Statement
There was no funding nor financial support for this study.

_t-scan_data_with_a_balanced_orthotic._b)_t-scan_data_representative_of_the_habitual_bit.jpg)








_t-scan_data_with_a_balanced_orthotic._b)_t-scan_data_representative_of_the_habitual_bit.jpg)