INTRODUCTION
An understudied and underserved aspect of dentistry is the complete lack of any measurement of the quality of masticatory function of routine dental patients. All patients need to be able to masticate effectively for good nutrition and to avoid such conditions as Irritable Bowel Syndrome, choking on food and other system disorders.1 While a lot of attention has been placed upon the TMD patient with pain, too often the patient unable to masticate properly has been left without options and ignored. For more than three decades researchers have pursued the development of methods for analyzing masticatory movements as a means of detecting malfunctions of the system.2–4 The first major break though was the concept of calculating the Averaged Chewing Pattern (ACP), including a very large sample of normal control subjects (500) without any indications of malfunction, as well as many subjects with all of the common types of internal derangements of the TMJ.5
Originally, the only purpose of calculating the ACP was to detect the presence of internal derangements of the TMJs in a clinical setting.6–11 In one study an artificial neural network was trained to differentiate specific TMJ internal derangement conditions.12 Previously, the detection of reversed chewing cycles had been found to coincide with posterior crossbites,13,14 and cusp to cusp relationships, while occlusal interferences were shown to alter the mastication pattern.15 Recently, it has been clarified that in very young subjects with primary dentitions the reversed chewing cycles are common since they are still learning how to use their dentitions, which are also in a state of flux.16 Children also exhibit greater variability, less smoothness and faster cycle times than adults.17 Normal adult subjects have been shown to use a consistent chewing pattern over time.18 However, the biggest benefit has been the establishment of which parameters can describe a normal chewing pattern.5
Cycle times that are less than 800 milliseconds in mean duration, opening and closing times that have standard deviations of less than 50 milliseconds and ACP vertical values of 10 to 22 mm indicate good function. When accomplished with normal muscle activity it is ideal. If accomplished with abnormal muscle activity, it is still an indication of successful adaptation.
The ACP method requires; 1) recording incisor-point movements in a non-interfering way while chewing, 2) segmenting the chewing sequence into individual cycles and 3) averaging the cycles into a mean 3-dimensional movement pattern that includes a mean velocity pattern.5 The ACP succeeds in characterizing a subject’s underlying chewing pattern because of the mathematical phenomenon that random movements within a chewing sequence are mostly canceled by the averaging of ten to twenty cycles, while consistent movements are retained by the averaging. The law of large numbers states that the larger the sample the more precise the average becomes. For incisor-point chewing patterns, the average tends to stabilize when 10 to 20 cycles have been averaged and adding additional cycles has little effect. However, the bolus used is critical because it plays a big part in the size, shape and other parameters of the pattern.19,20
Softened chewing gum is a popular bolus for testing because of its very chewable consistency, the fact that it is not consumed and the need for a reproducible bolus that does not itself change the pattern.21 However, chewing gum represents a kindergarten level test when compared to a harder, tougher bolus that is not consumed too quickly and is a better indication of a patient’s masticating ability. The tough bolus provides a more sensitive indication of a less substantial masticatory disfunction.
METHODS and MATERIALS
Source of data
This study was conducted in the Department of Prosthodontics and Oro-facial pain clinic of Rajarajeswari Dental College and Hospital, Bengaluru, during the years 2018-2020 with an aim to evaluate the masticatory efficiency and muscle activity in patients with and without treatment partial dentures in mandibular Kennedy’s class I situation.
The study population consisted of 35-55-year-old healthy asymptomatic subjects, selected from the Department of Prosthodontics at Rajarajeswari Dental College and Hospital, Bengaluru. All the subjects were examined and evaluated clinically. The inclusion and exclusion criteria were set to avoid any potential bias that could reasonably confound the interpretation of the results.
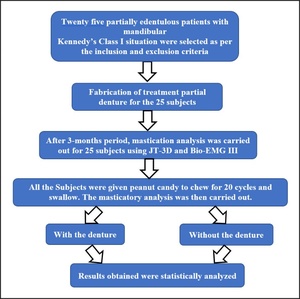
Thirty partially edentulous subjects with Kennedy’s class I situation were selected. These subjects had undergone recent extraction and had visited the hospital for the replacement of the missing teeth. The primary complaints among these subjects were related to poor masticatory ability. Each subject was provided with treatment alternatives like treatment partial dentures, cast partial dentures, and implant-supported fixed prosthesis. As the study was intended to evaluate the masticatory efficiency among the rural population using a treatment partial denture, the selected subjects were provided with treatment partial dentures.
All the subjects were informed about the study and procedure to be done and the details including name, age, gender, dental history were taken. All the selected subjects signed informed consent forms granting permission for their records to be used in research. The study was conducted after the subjects signed informed consent forms, and the dissertation work was approved by the ethical committee of Rajarajeswari Dental College and Hospital. Ref: RRDC&H/PG-07PROSTHO/2018-19.
Inclusion Criteria
-
Subjects within the age group of 35-55 years
-
Partially edentulous subjects – missing posterior teeth
-
Maxillary arch – fixed/removable denture
Exclusion Criteria
-
Subjects with systemic diseases affecting bone quality
-
Temporomandibular joint dysfunction
-
Compromised periodontal diseases
-
Over eruption of opposing teeth
-
Subjects with a history of muscle disorders
Fabrication of Treatment Partial Denture
Patients who reported to the OPD of the Department of Prosthodontics at Rajarajeswari Dental College and Hospital were clinically examined and the subjects were selected based on the inclusion and exclusion criteria. The subjects were explained about the study and an informed consent was signed by them before starting the procedure. All the 30 subjects underwent the standard treatment protocol procedures required for the fabrication of a treatment partial denture.
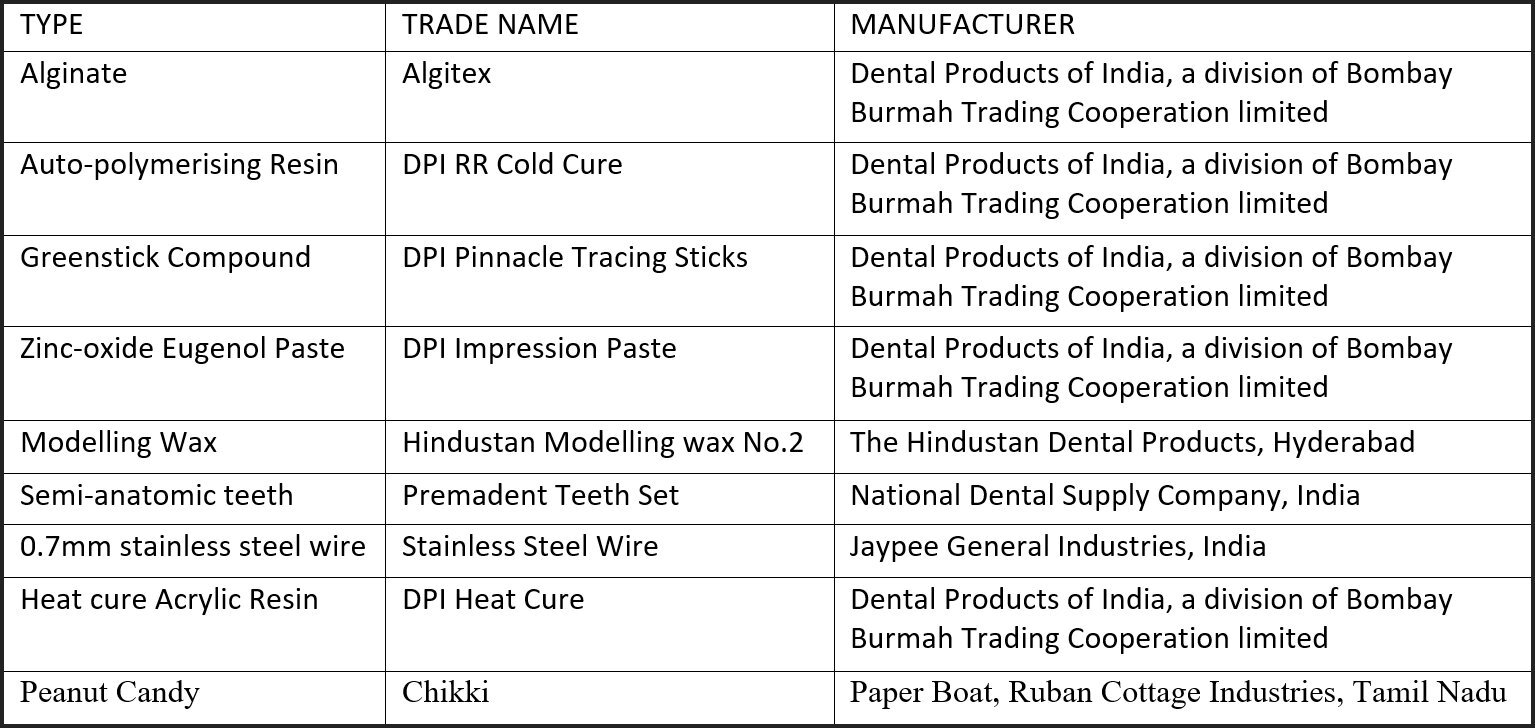
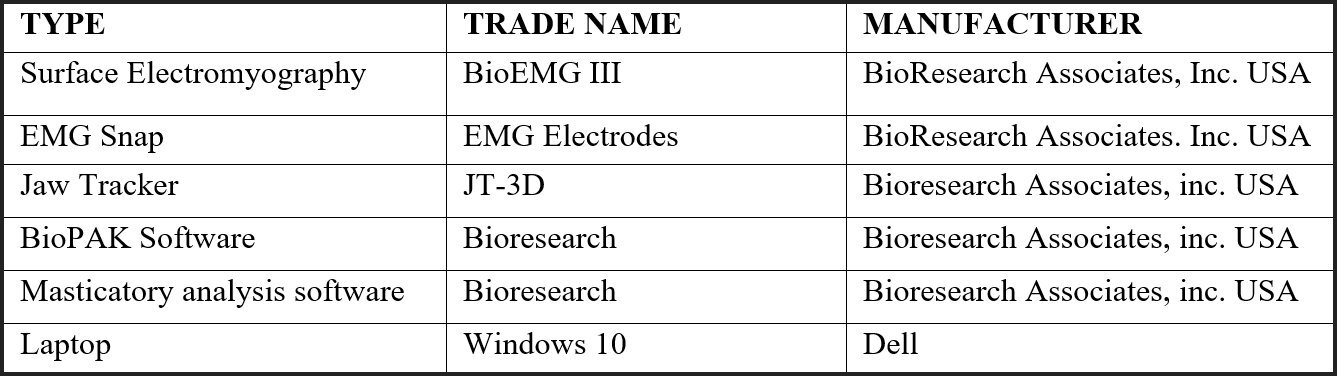
Materials consumed are listed in Figure 1. The Biometric equipment used is listed in Figure 2. Additional tools and supplies used for treatment are listed in Figure 3.
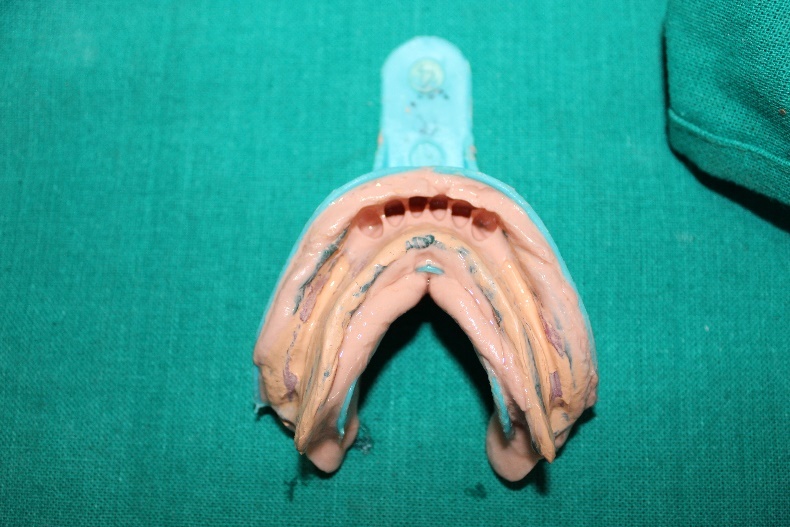
During the first appointment, stock trays of adequate size were selected to make maxillary and mandibular arch impressions using alginate and the primary casts were poured using dental stone. A custom tray was fabricated using auto-polymerizing resin on the lower cast which was kept 2mm short of the borders. Border molding was carried out using a green stick and zinc-oxide eugenol paste was used to record the tissues based on the mucostatic principle. A final impression was made using Mc Lean’s technique. The final impression was poured using dental stone and a denture base with occlusal rim was fabricated for jaw relation procedure.
Face bow transfer was done using Hanau spring bow to record the orientation jaw relation. The occlusal rim was adjusted to the required vertical dimension and a softened wax was added over the rim to record the bite in centric relation and the casts were mounted on a semi-adjustable articulator (Hanau Wide-Vue II). Semi-anatomic teeth of 200 cuspal angulation were used for teeth arrangement in the established centric relation. The trial denture was evaluated in the subject before the fabrication of a final denture. Stainless steel wire 0.7mm thick was used to make retainers on the primary abutments. The final denture was fabricated using heat cure material using a compression molding technique. Finishing and polishing of the treatment partial dentures were done. During insertion, the occlusal corrections were carried out using T-Scan to remove any lateral interferences (Tekscan, Inc. S. Boston, MA USA).
The treatment partial dentures were delivered to the subjects. Post insertion instructions were given, and they were recalled after 24 hours as a standard insertion protocol for a removable prosthesis.
Masticatory Movement Analysis
Masticatory movement analysis was carried out to check the masticatory efficiency with and without the prosthesis. Three months from the time of delivery of treatment partial dentures, the subjects were recalled for a check-up. The muscle activity and masticatory efficiency were then evaluated using Bio EMG III and a JT-3D Incisor-point Tracker with BioPAK software (Table 2). The masticatory movement analysis included these significant aspects;
-
Shape of the chewing pattern
-
Size of the chewing pattern
-
Velocity of the chewing pattern
-
Timing of the chewing pattern
-
Variability of the chewing pattern.
Variability of the Muscle Activity
The Average Chewing Cycle (ACC) of the masseter and the temporalis muscles can be calculated by averaging the electromyographic (EMG) activity burst over a sequence of 10-15 chewing cycles. This process removes the random variation between individual cycles, reveals the underlying shape of the contraction pattern, provides a measure of variability and reveals the hierarchy of muscle activity between the four muscles. The Average Chewing Cycle of the muscles includes;
-
Normal activity effort levels exist - Working Masseter, Working Temporalis, Non-working Temporalis, and Non-Working Masseter.
-
Mean Area/cycle (contribution of each muscle)
-
Peak Amplitude (Maximum effort location)
-
Standard activity distribution (temporalis vs masseter)
-
Variability of muscle activity patterns
To carry out the masticatory movement analysis the subjects were taken to the Department of Oro-Facial pain clinic at Rajarajeswari Dental College and Hospital. The subjects were explained about the biometric tools. The subject’s skin was prepared using 70% alcohol to attach the surface electrodes. The electrodes were attached at the anterior temporalis and superficial masseter bilaterally as shown in Figures 4 & 5 along with an isolated reference electrode attached to the upper trapezius muscle, connected to the Bio-EMG III amplifier, but not to the computer. A computer program, BioPAK (BioResearch Associates, Inc. Milwaukee, WI USA), was included with the JT-3D incisor-point tracker to facilitate motion analysis. Figure 5.
The Electrognathography (EGN) headset was placed on the subject’s head and aligned to a magnet adhered to the mandibular incisors and/or gingiva in the labial vestibule, which sat well below the opposing maxillary incisal edges allowing for dental intercuspation and mastication without any contact of the upper incisors. Figure 5.
This set up recorded the muscle activity changes and the magnet’s changing path during repetitive peanut candy chewing. Peanut candy of a 2 cm by 2 cm standardized size was used for all the subjects because it is hard, stable, easy to chew, and reproducible in its characteristics, especially for repeated sessions. No instruction was given to any subject regarding the rate or intensity of chewing, but the side of chewing was specified to ensure unilateral chewing was recorded.
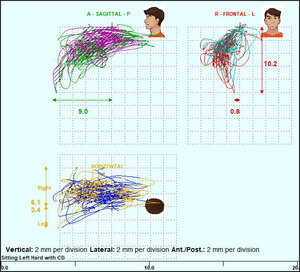
The subject was asked to hold the peanut candy between their tongue with their posterior teeth in light occlusion until the EGN and EMG recordings were activated. The subjects then chewed the peanut candy for 20 cycles solely on their left side, (Figures 6 & 7) after which the recording was stopped. The subject was given water to swallow the remaining peanut candy particles. A fresh peanut candy was given for their right-sided chewing and their second recording was activated, where the subject chewed the peanut candy for 20 more cycles only on the right side.
This process was performed without the treatment partial denture and then with the treatment partial denture resulting in the recording of two chewing sequences left-sided and two right-sided sequences per subject. See Figure 8. All the recordings were carried out by a single clinician, faulty recordings were discarded (magnet became loose, headset moved misaligning the array, electrodes dislodged from the face) and re-recorded.
Operational Flowchart
Each individual subject’s masticatory analysis data were obtained using the BioPAK Mastication software which forms the basic data of the study. See Figure 9.
-
Masticatory movement analysis without treatment partial denture using hard food on the right and left side.
-
Masticatory movement analysis with the treatment partial denture using hard food on the right and left side.
-
The data was subjected to statistical analysis and presented in the form of tables.
(Note: There are additional illustrations in the appendix.)
RESULTS
Motion analysis
Using the Mastication Module within the BioPAK program the chewing data were analyzed by comparing the pre-treatment movements to the same patients’ post-treatment measurements using Student’s paired t-test. The significant improvements in the left and right chewing parameters are shown in Table 1 and Table 2 respectively.
In the left-sided mastication motions there were significant reductions: a) in the mean closing time, b) in the variability of the mean antero-posterior Turning Point location, c) in the mean antero-posterior position of the Terminal Chewing Position (maximum bolus crush), d) in the mean maximum and average opening velocities, e) in the mean Frontal and horizontal closing angles and f) in the mean closing jerkiness. There was a significant and concurrent increase in the mean laterality of the terminal chewing position. See Table 1.
For the right-sided mastication movements there were significant decreases in; a) the mean cycle time, b) the mean lateral Turning Point, c) the mean lateral Terminal Chewing Position and d) in the mean opening velocity. Significant increases were found in; a) the mean antero-posterior Terminal Chewing Position, b) the mean variability of the lateral Terminal Chewing Position and c) the mean Frontal opening angle. See Table 2.
Muscle activity
Table 3 presents the mean effort that was expended in the masticatory EMG activity using the integrated EMG as a proxy (the area under the rectified/averaged chewing burst). When the subjects were chewing on the left side the amount of effort remained rather constant between pre-treatment and post-treatment. This is expected because the amount of effort is determined mainly by the texture of the bolus. This bolus was rather tough and required a substantial effort. Note: For a soft bolus, the extra effort required by a dysfunctional situation could reveal a significant difference after a treatment improved efficiency.
The coefficient of variation (SD/Mean) revealed that some significant differences were found; such that the variability of both the working and balancing masseter muscles were significantly reduced after treatment.
It was also revealed that the mean time from the peak of the muscular closing activity to the end of closure was significantly changed for the working temporalis and non-working masseter.
Table 4. presents the effort expended in the masticatory activity when chewing on the right side, also using the integrated EMG as a proxy. Within this data the working temporalis muscle did significantly reduce its activity after treatment, but the other three muscles remained constant as expected.
With respect to the variability of the EMG activity, the non-working temporalis was the only muscle to significantly reduce its variability. The masseters did reduce their mean coefficients of variability but did not reach significance.
The working masseter was the only muscle to significantly change its time from the peak EMG activity to the End of Closure. The other three muscles did not change their timing significantly.
Seven of the 30 subjects could not chew the bolus provided on the left side and four could not chew the bolus provided on the right side prior to receiving the treatment partial denture and had to be eliminated from the study. Thus, the sample for left-side mastication was n = 23 and for the right-side mastication n = 26.
DISCUSSION
The motion analysis revealed increases in the velocity of chewing and reductions in the variability. These changes were most often in the direction of values associated with fully dentulous (asymptomatic) subjects.6–11 The somewhat different results from the left-sided and right-sided chewing should not be surprising since each side has its own occlusal and functional characteristics.
Nine of the 34 available parameters for left-sided chewing and seven of 34 for right-side chewing revealed significant changes after treatment. See Tables 1 & 2. Although there were nine and seven significant parameters for left and right chewing respectively, they weren’t all the same parameters. This occurred because each side has its own characteristics and because the size of the sample may have been marginal. Some of the available parameters, although showing trends, failed to reach significance, also likely due to the very high variability of the pre-treatment data.
The fact that the significant differences were not the same for left and right mastication illustrates that asymmetry is prevalent within the human masticatory system. A larger sample may have resulted in more agreement between the data from the left and right-side masticatory motions. Each chewing parameter is affected only by specific factors like occlusion, TMJ function, maxillo-mandibular relationship, etc. It is only for a worst-case scenario that a larger number of the parameters are found to be abnormal.
Since dysfunction tends to increase the variability of muscle function, the EMG data were analyzed for any changes in the amount of effort as well as for changes in the variability of the effort and the timing of closure.11 The only significant change in the mean chewing effort was for the working temporalis, which showed a significant decrease after treatment when masticating on the right side. The required chewing effort is mostly a function of the texture of the bolus and tends to affect the temporalis more than the masseter in normal control subjects.22–24
Significant changes in variability were seen in two muscles during left-sided mastication and one muscle in right sided mastication. These changes could be attributed to a more organized approach to chewing with the treatment partial denture in place. See Figures 6 & 7. In contrast, previous studies have shown consistency between successive sessions in the individual mastication of subjects without removeable prostheses.24–27
An example of the pre-treatment and post-treatment muscle activity patterns are shown in Figure 10AB. In Figure 10 A) the mean peak EMG activity occurs in all the muscles after the End of closure (maximum bolus crush). The highest peak activity in this sample patient is recorded from the non-working left anterior temporalis muscle. In Figure 10 B) after the delivery of the treatment partial denture, the peak EMG activity occurred in all but one muscle (the working masseter) prior to the End of Closure, which is the more normal condition.28 The highest activity switched from the non-working anterior temporalis to the working anterior temporalis muscle, also a more normal activity pattern.28
In six out of eight muscles the mean time from the peak activity to the end of closure increased, in three of those it was significant (p < 0.05). Prior to treatment four of eight muscles included negative values, indicating that the peak occurred after the end of closure. This is an abnormal condition that reflects hesitancy on the part of the subject and is seen in patients with masticatory dysfunction.28
LIMITATIONS
The reduced number of samples from thirty to 23 and 26 for left and right mastication respectively may have caused some of the measured parameters to not reach significance. Missing posterior teeth should be an obvious handicap and interfere with a subject’s ability to masticate. However, there are so many factors that affect a subject’s ability to masticate and the combination of factors can be different for every individual. Thus, a larger sample may be required to fully eke out the most relevant factors involved.
CONCLUSIONS
The delivery of a treatment partial denture appeared to significantly enhance the masticatory function of this group of subjects. Several specific reductions were noted in variability of both the motions and the muscle activity producing them. A more organized pattern of movement and improvements in the timing of muscle contractions were also noted. A larger group of subjects will be needed to definitively delineate the significance of each parameter.




_post-treatment_left_chewing_with_removeable_treatmen.jpg)

_the_average_chewing_cycle_(acc)_of_the_muscle_activity_with_the_peaking_occurring_afte.jpeg)









_post-treatment_left_chewing_with_removeable_treatmen.jpg)


_the_average_chewing_cycle_(acc)_of_the_muscle_activity_with_the_peaking_occurring_afte.jpeg)