Introduction
Patients who present with opposing canines that do not occlude, or have shallow guidance exit angles are predisposed to living in an occlusal state that contains excess occlusal surface friction present in their right and left excusive movements. From a functional perspective, these missing canine contact, edge-to-edge, or shallow canine guidance patients (Figures 1 & 2) present with limited or no vertical canine overlap (or anterior vertical overlap), such that no vertical lift occurs during excursions that could separate their posterior teeth.
As the mandible moves laterally without lift, the working side premolar and molar teeth engage and continue to contact as the mandible moves laterally away from MIP (Figure 3). This same lack of vertical excursive lift and posterior excursive engagement also occurs in patients who have worn guidance teeth, with sanded away incisal edges (Figure 4). Any lack of anterior excursive lift always predisposes the patient to have posterior working and balancing interfering contact in their excursive functional movements.
Bonded composite has been employed in clinical practice mostly for esthetic smile corrections, like adding contour to worn incisal edges or closing diastemas.1–5 Alternatively, Guidance Enhancement with direct composite is a previously described method to create absent canine contact before performing a Disclusion Time Reduction procedure.6 Composite can be employed in slight to moderate open occlusion cases where opposing canines are near enough to each other, that they can be occluded with composite without compromising the anterior tooth shape esthetics (severe open occlusion patients are a contraindication).6 Regardless of whether a patient presents with a slight anterior Open Occlusion, a slight lack of canine contact in MIP, or shallow anterior guidance, the clinician will need to visualize which parts of the canine teeth can be used to build in anterior guidance contact(s), to increase the vertical guidance lift angle for improved posterior disclusion.
Multiple published T-Scan/EMG studies since 1991 have repeatedly documented that excursive functional interferences, group function working side guidance, and occlusal surface excursive movement frictional contacts are etiologic factors for muscular pain and symptoms observed commonly in TMD patients.7–24 Excursive occlusal surface friction directly elevates masticatory muscle activity levels via the neuroanatomy and neurophysiology of the PDL mechanoreceptors and the posterior tooth pulpal fibers.25 This elevated ongoing muscle activity is a known contributor to many chronic symptoms that fall under the TMD umbrella.7–24 When an occlusion lacks anterior vertical excursive lift, patients produce higher than physiologic, excursive movement muscle contraction levels, making a lack of effective anterior guidance an etiologic component in an open canine contact patient that develops a muscular TMD condition.
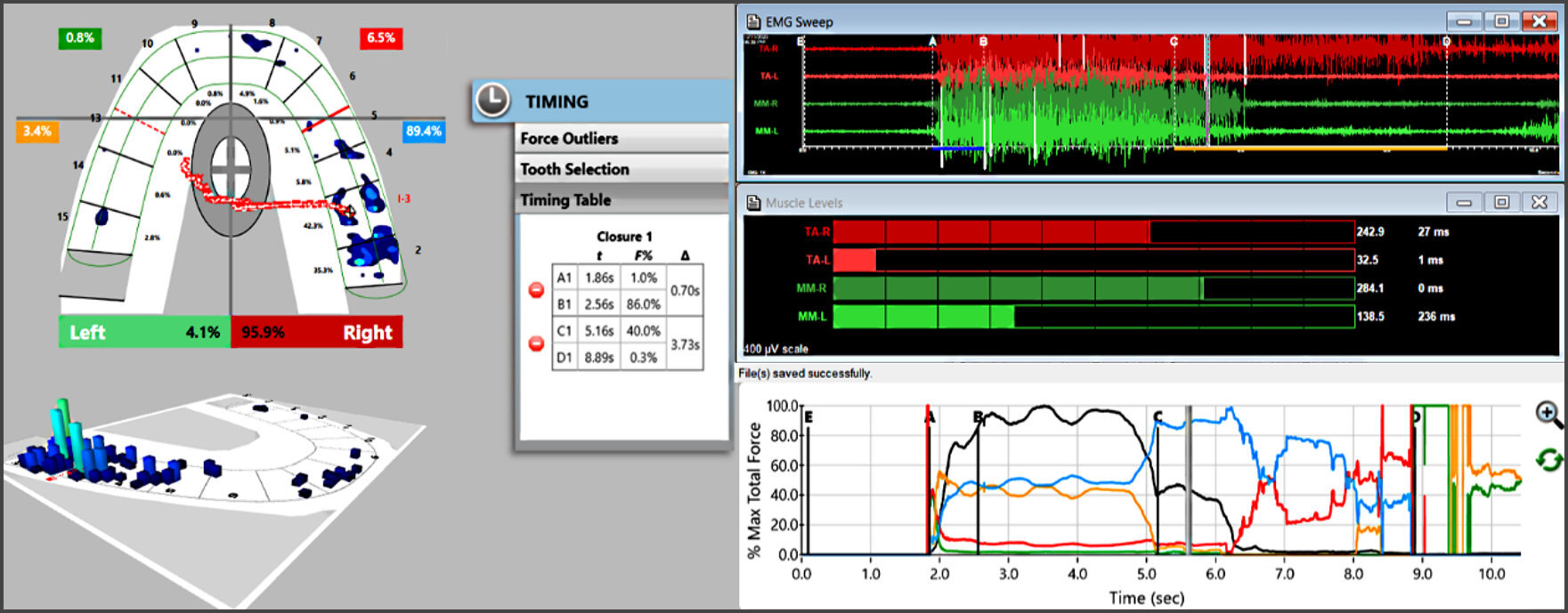
Resolution of the high muscle firing and common chronic muscular TMD symptoms has been repeatedly treated successfully by the measurement-driven, computer-guided occlusal adjustment procedure known as the Immediate Complete Anterior Guidance Development coronoplasty (ICAGD).13,26 ICAGD coronoplasty measurably decreases the time required for all molars and premolars to disclude from each other (known as the Disclusion Time) in ≤ 0.4 seconds during right and left mandibular excursions commenced from complete intercuspation in Maximum Intercuspal Position (MIP).26 ICAGD has specific time-duration, numerical endpoints that must be achieved to verify the coronoplasty was properly accomplished,11,18,24 which is guided by two synchronized technologies; the T-Scan 10 occlusal analysis system, (Tekscan, Inc. S. Boston, MA, USA) and the BioEMG III Electromyograph and BioPAK software (Bioresearch Assoc., Milwaukee, WI, USA).16–18 Together, they simultaneously record real-time force movies of mandibular excursive movements, and those same movements’ associated masticatory muscle contraction patterns. ICAGD can be used to treat Occluso-muscular pain symptoms without a required splint, appliance, or deprogrammer7–24 and can be directly rendered in patients with existing canine contact bilaterally. However, if one or both canines do not couple the degree of open canine contact will direct treatment, whereby either tooth movement orthodontically or creating canine contact prosthetically must precede shortening the Disclusion Time with ICAGD.6
This Case Report describes a female dentist with chronic temporal headaches and jaw pain, that presented with open canine contact, worn canine guidance surfaces, and bilateral working side group function guidance. She was treated with a right-sided bonded canine addition, and a left-sided bonded canine-lateral addition, that were immediately followed by the ICAGD coronoplasty. In the treatment appointment, the patient’s pre-treatment high excursive muscle firing was markedly lessened, and shortly thereafter, her 20+ year-long chronic headaches and jaw symptoms readily abated.
Case Report
A 42-year-old female dentist presented with complaints of 20±year long history of chronic headaches behind her eyes, that came on in the middle of orthodontic treatment she underwent years prior. The orthodontist suspended treatment and left the town he was practicing in, leaving the patient at age 16 with incomplete anterior coupling. At her initial occlusal and muscle evaluation in 2020, the patient reported that in her 20s she stopped chewing gum as her muscles would quickly become sore. In addition to suffering with chronic temporal headaches, the patient often wakened clenching into her night guard (used for 10 years), and noticeable soreness on teeth #s5 and #19. She experienced intermittent left sided clicking and popping, sensitivity when drinking cold liquids, and occasional ear ringing and dizziness. The patient reported that if she did not wear her appliance, she would have definitive morning masseter soreness.
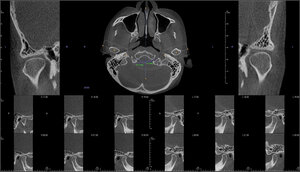
The patient’s CBCT (Figure 5) depicted in all slices, completely contiguous condyles that were fully corticated, normal skull base structures, and definitive disc space medial, posterior, and superior to both condyles. Her vertical mouth opening = 45 mm, indicating the visible TM Joint anatomy had a normal Range of Motion.
The intraoral examination revealed her occlusal plane was canted slightly to the left side with open canine/lateral contacts, and contacting canines on the right side, but tooth #6 had a worn incisal edge (Figure 1). When the patient excursed lateral
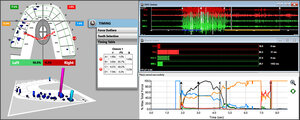
to the right or left, only posterior group function contacts engaged and controlled the movements (Figures 3, 4) (the Protrusive movement is not shown for brevity). The patient’s occlusal force distribution, excursive movements, and her masticatory muscular contraction patterns were recorded simultaneously with the T-Scan10/BioEMG III synchronized technologies. The patient intercuspated firmly into the T-Scan recording sensor (Novus HD, Tekscan, Inc. S. Boston, MA USA), held her teeth in Maximum Intercuspation (MIP) for 1-3 seconds, and then glided left out to towards her non-contacting canine teeth, with EMG leads in place on her masseter and temporalis muscles. The right excursive recording was made in the same fashion (Figures 6, 7).
This functional assessment confirmed the right and left Disclusion Time values were outside of the known physiologic ranges (DT ≤ 0.4 secs.)16,18,24 (3+ seconds in both excursions), which caused high levels of excursive muscle firing that contributed to the patient’s longstanding headaches and jaw pain. The patient did not want to undergo a lengthy course of orthodontic treatment to couple her left canines, but instead consented to immediate coupling with bonded composite additions to the maxillary left lateral incisor and canine, and to adding guidance lift to the right canine incisal edge. The bonding process created functional anterior guidance surfaces that would control the patient’s new right and left excursions (Figures 8-12) that safely would allow the patient to undergo ICAGD with minimum reductions made to the posterior interfering occlusal contacts.
Guidance Enhancement Procedure
Surface and mechanical retention was created for the bonded additions (Figures 8 and 9). The etchant (Select HV 35%, Bisco, Schaumburg, IL, USA) prepared the enamel, followed by unfilled bonding resin (Optibond SoloTM Plus, Kerr Corp., Orange, CA. USA), and then composite (FiltekTM Z250, 3M ESPE, St. Paul, MN, USA) was tacked onto the incisal edges, and the facial and lingual retentive surfaces of #s 6 and #s 10, 11 (Figure 10). It was formed and shaped by paintbrush and hand instrument, to render an appropriate esthetic shape. Extra composite bulk was placed on the lingual aspects of the addition, so that definitive contact would be made with the opposing lower tooth (which was brushed with glycerin as a separator). Before curing the new addition, the patient was instructed to fully close into her MIP position, and keep her teeth firmly intercuspated during the curing process.
The lower canine(s) penetrated the extra bulk and formed the ideal functional shape of the addition’s guidance ramp, to exactly match the outer facial-incisal shape of the lower canine without changing the patients Vertical Dimension. Curing was completed first with all teeth in MIP, and then again after all teeth were separated to access the lingual composite and its’ area of retentive enamel (Figure 11). The excess composite was then removed and the final esthetic shaping of each addition was perfected (Figure 12). The patient tested their new guidance surfaces by sliding across them with articulating paper interposed. Minor functional adjustments were made to improve the ease of sliding laterally.
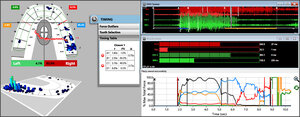
There was no vertical lift present in each excursion, that could be used to disclude the posterior teeth. So, a new set of T-Scan/BioEMG III right and left excursive recordings were made to assess each bonded addition’s functional excursive improvement, and their impact on the excursive muscle activity levels, before any changes were made to the posterior teeth (Figures 13, 15). Neither added guidance surface completely discluded the working side posterior teeth (Figures 14, 16), but did somewhat lessen the pre-bonding elevated excursive muscle activity levels.
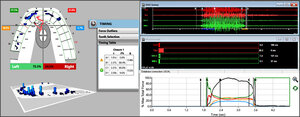
Next, the ICAGD coronoplasty was performed on her right and left excursive movements as previously described,26 controlled by the new bonded guidance surfaces. The corrective adjustments removed the remaining occlusal surface friction and reduced the DTs to within physiologic limits. Post ICAGD, new left excursive and right excursive movements recordings were made in a fashion similar to pre-ICAGD (Figures 17, 18).
The post-ICAGD right excursive DT = 0.35 seconds (Figure 17), and the post-ICAGD left excursive DT = 0.22 seconds (Figure 18). Compared to the both the pre-bonding excursive EMG hyperactivity (Figures 4, 5), and to the bonding-only EMG data (Figures 13, 15), the post ICAGD
The patient was followed up after the ICAGD procedure, when she reported significant reductions in headache frequency and severity. She was advised to reappoint for follow up appointments to help make minor T-Scan guided excursive muscle activity levels were dramatically lessened (Figures 17,18). Figures 19, 20 & 21 show the completed bonded guidance surfaces in place providing visible posterior excursive disclusion corrections to aid in her adaptation to both her new guidance surfaces, and to any changes in her overall occlusal function.
Discussion
The clinical outcome of this Case Report aligns very closely with the numerous published papers that have described the rapid physiologic healing effect that Disclusion Time Reduction offers myogenous TMD sufferers.7–24 This patient’s response to adding in bonded guidance surfaces that ensured that rapid excursive posterior contact disclusion timing was achieved, and then discluding the patient measurably on those bonded surfaces, mirrors that which has been reported in many published ICAGD studies and Clinical reports7–24 in the literature since the late 1980’s. This Case Report is another example illustrating that muscular TMD symptoms, jaw pain and temporal headache respond well to anterior-excursively-controlled, precise, time-measured occlusal adjustment therapy.
ICAGD (directly by itself where applicable, or in combination with Guidance Enhancement) lessens hyperactive muscles from within the Central Nervous System (CNS), by controlling the molar Periodontal Ligament (PDL) mechanoreceptors and pulpal nerve fibers, which synapse directly with efferent motor fibers that contract the four masticatory muscles, and the Swallow Mechanism muscles.25 Prolonged excursive frictional contacts increase the total time the pulp is flexed and the PDL mechanoreceptors are compressed during excursive movements.
Both the pulpal flexure time and the PDL compression time is equal to the Disclusion Time duration of that same excursion.13,16,18 Prolonged durations of periodontal and pulpal fibers activation, result in prolonged durations of masticatory muscle contractions.13,16,18 By reducing the length of time the posterior occlusal surfaces contact excursively, the duration of pulpal flexure and PDL mechanoreceptor compressions are reduced, interrupting the muscle hypercontraction. Post ICAGD, the pulp and PDL no longer hyperfunction the involved muscles into a painful ischemic state, allowing for re-oxygenation and muscle fiber recovery, leading to symptom resolution.
Although the traditional roles of bonded composite have been to improve smile defects, cover discolored enamel flaws, add shape and contour to worn anterior teeth, close diastemas, and with stronger types, to fill posterior teeth instead of amalgam,1–5 anterior Guidance Enhancement to pre-improve excursive movements for DTR Therapy, is an important application of the composite materials. The possibility of readily adding in missing guidance surfaces, or steepening worn out guidance surfaces, quickly can alter a poorly functioning occlusal scheme with compromised anterior guidance and high excursive muscle firing, into one that can be readily treated with ICAGD to remove that high excursive muscle firing. Long term due to material wearability,1–5 the composite additions should be changed out for porcelain veneers.
As this clinical case illustrated, the bonded additions alone will not produce the physiologically least possible amount of excursive muscle activity, as canine-canine contact generally provides inadequate posterior disclusion for optimal neuromuscular physiology. This was seen in the post bonding T-Scan/BioEMG Figures (Figures 11, 12 and 14, 15). Only by following the bonded additions with ICAGD were the lowest possible levels of muscular activity clinically achieved (Figures 17 and 18). Therefore, the neural output from the posterior teeth that causes muscle hyperactivity and muscular symptoms, can only be successfully muted neurologically by controlling the time-durations posterior teeth frictionally engage.
Funding statement
No funding was received from any institution or funding agency for this Case Report study.
Conflict of Interest Statement
No conflict of interest was reported by the author.

_and_concave_(tooth__11)_guidance_surfaces_tha.jpeg)



.jpeg)











_and_concave_(tooth__11)_guidance_surfaces_tha.jpeg)





.jpeg)











