Introduction
The Occlusion literature has demonstrated repeatedly that an occlusion with balanced bite force and short disclusion times can result in a myriad of functional improvements, including increased range of motion, reductions in clicking and popping of the Temporomandibular Joints (TMJs), improved mastication, reduced cold tooth sensitivity, relaxation of hyperactive muscles, and reductions in Beck Depression Inventory scores in chronic pain patients.1–6 Recently, a growing interest in posture as it relates to occlusion, is under scrutiny.
Posture is the active state of body support during the course of muscular activity, or as a result of coordinated actions executed by a group of muscles to maintain stability.7 “One of the most common faulty postures of the cranio-cervical region is forward head posture (FHP).”7–9 Moustafa et al., reported FHP negatively affected cervical sensorimotor control and the autonomic nervous system, while demonstrating a strong correlation between cerebrovascular accidents (CVA), and both sympathetic skin changes and cervical sensorimotor changes.10 Interestingly, greater sway was also detected in subjects with forward head posture, than in matched controls with normal head posture. FHP geometrically increases the perceived weight of the head.11,12
Mammalian animal studies help researchers understand neurophysiology that cannot be ethically researched in humans. Occlusal alterations in mammals caused deleterious effects in dogs and rats.13,14 Rats with composite fillings placed on their right 1st maxillary molar, deviated rat mandibles to the left and increased the right-side bite force. When radiographed to examine the composite’s effect on vertebral alignment, visible wry neck phenomena, and scoliotic spinal curvatures were both detected. Some of the rats twisted to the right (Figure 1)13 and others twisted left (Figure 2).13 After placing the same size composite on the left 1st maxillary molar to restore balance to the bite, 83% of the rat spines self-corrected and realigned normally.13 In a dog study, Sumioka purposefully ground down dog teeth unilaterally that resulted in abnormal involuntary bodily movements, while symptoms of autonomic failure were observed.14 This unilateral occlusal destruction led to tremors, lameness, and abnormal posture.14 The author concluded the trigeminal nuclear complex not only contains the functions of the sensory relay to the face and controls chewing movements, but likely modulates motor control of the autonomic system, especially postural control.15
Robin was first to describe an interplay exists between occlusion and posture.15 Since then, several authors have come to this same conclusion, that occlusion plays a role or otherwise influences posture.16–29 However, the available literature does not support a cause-and-effect relationship between occlusion and posture, despite that strong correlating data shows occlusion can affect posture. Much of the inconsistency can be explained by differences in study design and differing metrics that were used to analyze the gathered study data. This study attempted to overcome these posture and occlusion research design compromises, by recording with the T-Scan 10 technology (Tekscan Inc. S. Boston, MA USA) the occlusal force distribution data and occlusal contact timing data, with companion sway and postural data recorded with the MatScan technology (version 7.80, Tekscan, Inc. S. Boston, MA, USA), in muscular TMD subjects, before and after having their excursive Disclusion Times and bite force imbalances treated with the T-Scan-guided ICAGD coronoplasty.30–32 ICAGD removes excursive contacts selectively until the Disclusion Time ≤ 0.5 seconds in right left and excursion. This Disclusion Time Reduction (DTR) has been shown repeatedly to successfully treat chronic Occluso-muscular TMD symptoms.1–6,30–32
Methods
The treated group consisted of 83 consecutive patients that presented to a dental practice seeking occlusal treatment to resolve their chronic TMD symptomology which included numerous symptoms such as myalgia and cephalgia. The group consisted of 63 female and 20 males. All included patients gave their HIPPA consent to a) participate in this research protocol, b) undergo ICAGD and DTR treatment, and c) allow their images to appear in a manuscript, by signing an Informed Consent document.
Posture
Standardized posture photos were taken within the Posture Screen Mobile APP pre and post DTR therapy, on the same day the patients underwent initial treatment. Each patient was asked to stand with their hands at their sides, without being given instructions to “relax” or “stand up straight.”
Postural changes detected in the pre and post DTR treatment photographs were analyzed with Posture Screen Mobile (version 11.2, Posture Co, Trinity, FL, USA), which is a posture assessment App that has demonstrated strong rater reliability and evidence of construct validity in both clinical and research settings.32
The program prompts the user to enter the subject’s height and weight, and to place key markers on their posture photos. The program then calculates an estimated head weight and position, where the more forward the head posture is, the heavier the head feels to the person.
Sway and Center of Force
Sway and Center of Force data was recorded pre-and post-ICAGD treatment, using the Matscan Force Platform at a recording sampling rate = 100 HZ, for a duration of 30 seconds. Subjects’ postural sway was recorded according to the International Standardization Committee put forth at the 2009 International Society for Posture and Gait Research Symposium (ISPGR).33 A foot template ensured constant and uniform podal input was captured during the sway recordings,17 because changing foot positions inevitably change sway.34 Each subject stood upright on the Matscan, with their teeth together in the foot template with their eyes closed for 30 seconds. Sway testing with closed eyes has been found more reliable than with eyes opened.17,35
The unmatched control group consisted of 32 patients that were seeking help for their TMD symptoms. These patients had the same occlusion, posture, and sway records recorded like the treated subjects, twice on the same day before and after their TMD consult. But no control subjects underwent the ICAGD treatment.
The Immediate Complete Anterior Guidance Development coronoplasty (ICAGD) procedural steps have been previously described by Kerstein,30 but are outlined below.
After air-drying opposing maxillary and mandibular quadrants, the patients were instructed to self-close into their maximal intercuspal position (MIP) with 20 micron articulating paper (Accu-Film II®, Parkell, Inc., Edgewood, NY, USA) interposed between the teeth on one side of the mouth. Next, the subjects excursed right towards the tip of the canine and then back into MIP, then left towards the tip of the canine, and then back into MIP. These movements marked all working and non-working interferences responsible for long Disclusion Times. These patient excursive movements were not guided or controlled by the clinician in any way.30
Then, on the side just marked, the clinician removed any inclined plane linear contact markings and refined all broad centric stops into tiny pinpoint occlusal stops, to leave only central fossa, cusp tip, and marginal ridge nonlinear contacts. After the first set of paper markings were adjusted, the patient was instructed to repeat the same mandibular excursions to remark the same two quadrants, after which similar adjustments were performed again. This process was repeated until no linear contact marks remained and visual disclusion had been achieved in both the working and balancing movements on that initial side of the mouth, within 1-2 mm of leaving MIP.30 The same marking and adjustment process was repeated on the opposing side.
Following bilateral ICAGD adjustments guided by successive T-Scan/BioEMG recordings, further patient self-closure into MIP and excursive movements were made, and refinement adjustments were performed until measurable short Disclusion Time was achieved in each excursion (DT ≤ 0.5 sec.), and measurable short Occlusion Time was achieved during patient self-closure into MIP (OT ≤ 0.2 sec.). Also, all force outlier contacts were treated, bilateral arch time simultaneity was established, and right-to-left occlusal force balance = 50% right-to-50% left +/- 5%, was created.30
All patients were treated at their existing vertical dimension of occlusion (VDO) in their existing maximum intercuspation position (MIP), purposefully forgoing mandibular manipulation to Centric Relation (CR), any myo-centric positioning via TENs or a swallow bite. After ICAGD was completed, each patient had their posture reassessed with the Matscan and Posture Screen Mobile, with any physical changes statistically analyzed with the Wilcoxon Signed-Rank test.
Results
Disclusion Times
All treated participants had their Disclusion Times reduced effectively (p<0.0000). Changes are reported in Table 1.
Sway Parameters
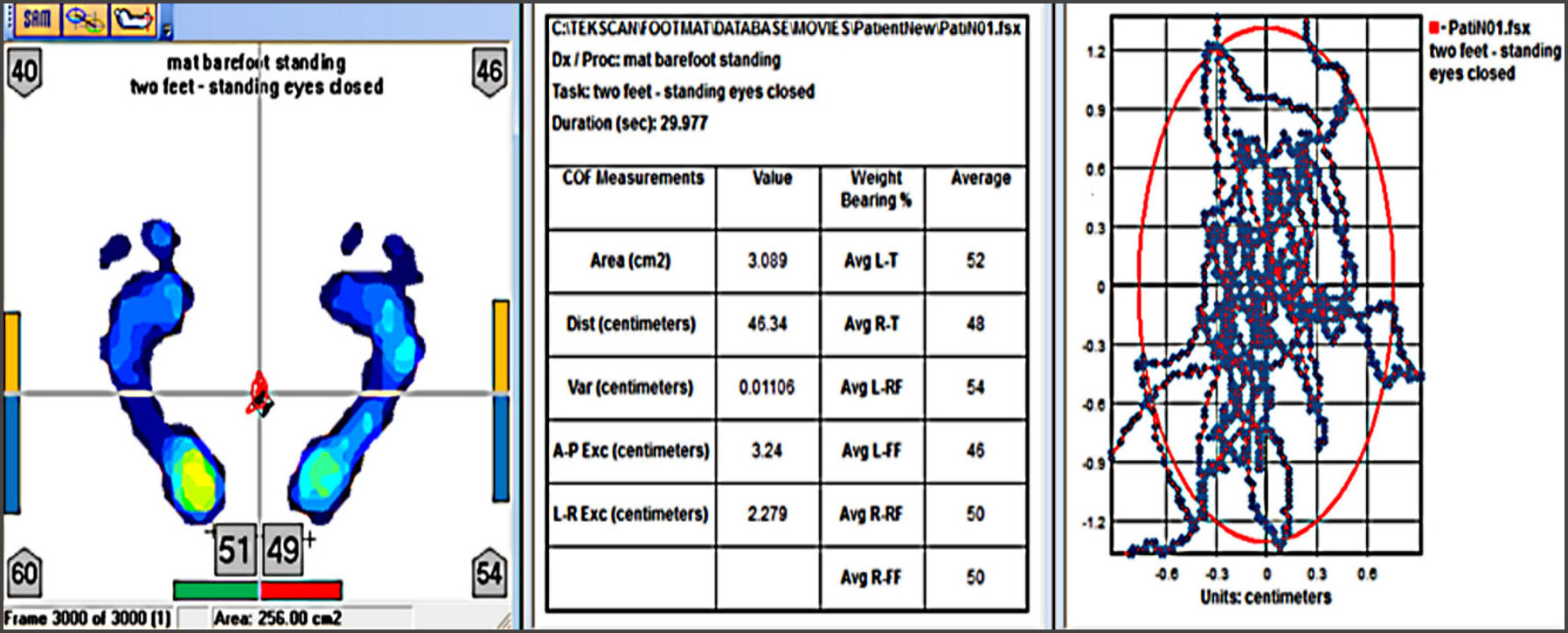
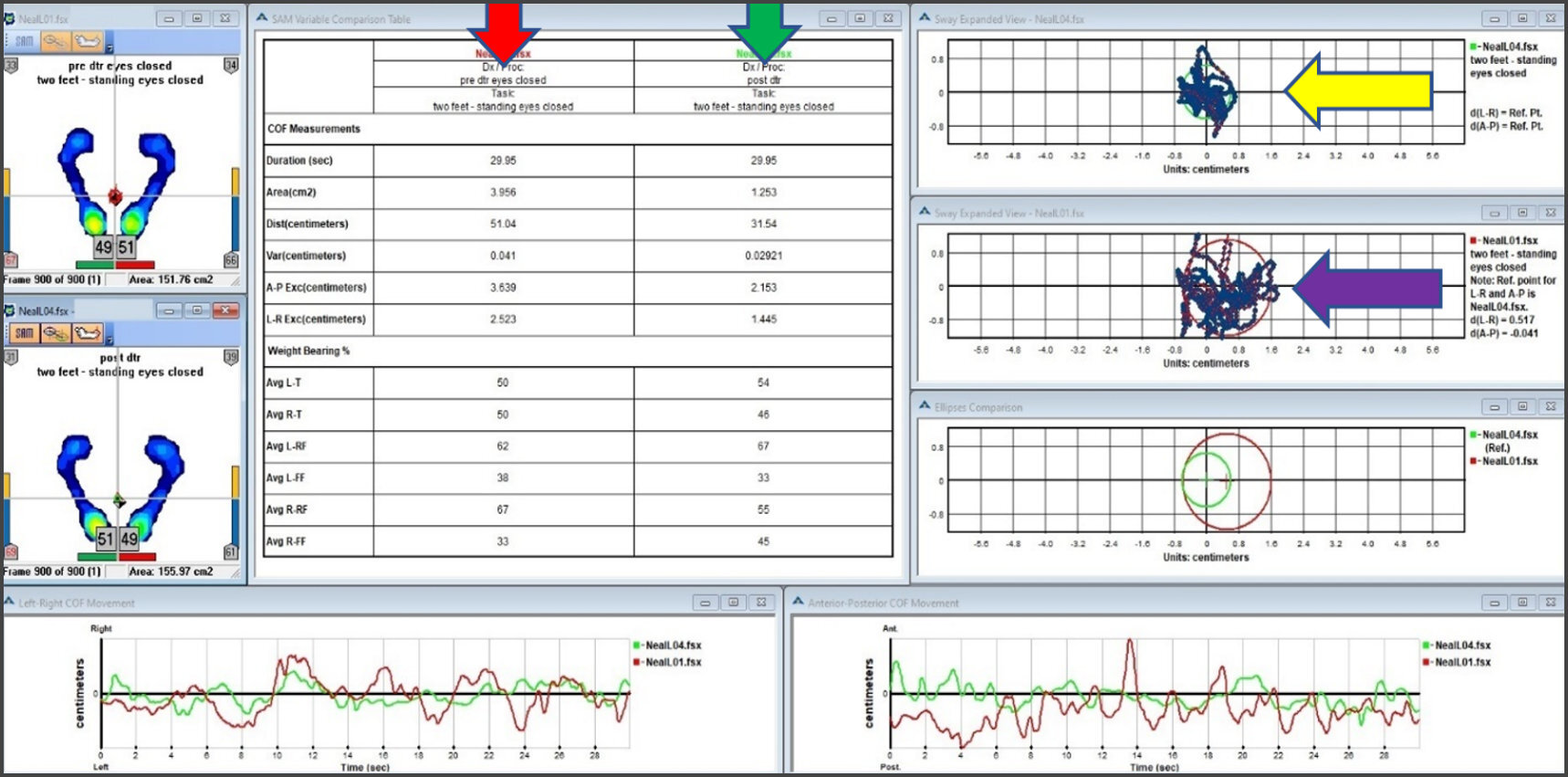
The specific Sway Parameters MatScan records include Area (cm2), Distance (cm), the antero-posterior (A-P) excursion (cm), and right and left (R-L) excursion (cm) (Figure 3).
Stability testing in the treatment group showed statistically significant improvements in all four Sway parameters pre to post ICAGD (p < 0.05) (Table 2), indicating the preexisting occlusion impacted the treated subjects postural Sway, and that ICAGD treatment reduced the amount of their Sway. It is known and accepted that reduced Sway corresponds to improved overall body stability.36
A minimal variation of estimated head weight was observed before to after consult in the control group (Table 3). This change was considered to be a random variation, not related to the consult since head weight was an estimate and not a measurement. The controls were also TMD patients exhibiting FHP, but not yet treated. Since their posture was not stabilized, the change was most likely due to physiologic variance.
The estimated head weights between the control subjects (34.0 +/- 10.43 lbs.) and the treated subjects before they underwent ICAGD (35.7 +/- 11.77 lbs.) were not significantly different. (Table 4).
The Sway Area parameter corresponds to the movement path of the Center of Force (COF) icon that summates the A-P and L-R movement ranges for the entire 30-second-long Sway recording. Greater area corresponds to greater Sway and less postural stability. A statistically significant reduction in Sway Area resulted post-ICAGD (2.00 cm2), compared to the subjects’ untreated habitual occlusion (3.62 cm2) (p < 0.00000).
The A-P Exc and L-R Exc parameters represent the antero-posterior excursion (front to back) and left-right excursion (side to side) measured in cm. An increase in either contributes to destabilized upright posture. After treating the occlusion with ICAGD, the A-P Exc significantly reduced from 3.90 cm to 2.39 cm (p < 0 0027), and the L-R Exc reduced from 2.18 cm to 1.52 cm (p < 0.00000).
The Sway Distance parameter (reported in cm), represents “how far” the COF icon wandered during the sway recording. After treating the occlusion with ICAGD, the Distance significantly reduced from 40.14 cm to 31.51 cm (p < 0.00000).
There were no significant differences in the Area, Distance or L–R values for the pre-to-post-consult within the control subjects (Table 5). Only the A-P Excursion slightly significantly decreased (mean control group decrease = 3.66%; p < 0.0016). 24 controls’ A-P sway decreased (mean decrease = 4.72% +/- 0.20,) while 8 slightly increased (mean increase =1.16% +/- 0.14). This small (unexpected) significant decrease was due to consistency of change rather than amplitude, as 75 % of the subjects all changed in the same direction (decreased). The control L–R was the second largest sway change, but it did not reach significance because nearly equal numbers of control subjects L-R increased and decreased.
Forward Head Posture
Statistically significant FHP changes occurred in the treatment group after ICAGD (Table 4), with the mean head position change = 0.58 +/- 0.37 inches, ranging individually from small improvement (0.07 inch) to sizeable (1.37 inch). These reduced forward head postures significantly reduced the estimated mean head weight from 35.7 +/- 11.77 lbs. to 28.9 +/-10.6 lbs. (p = 0.00001).
Table 6 shows the estimated mean head weight change resultant from forward head posture improvements pre to post ICAGD. The head weight reduced as the head self-up-righted. The smaller post ICAGD standard deviation indicated the variation of individual head weights was reduced after ICAGD.
Figure 4 shows a representative treated subject 's posture photos and body translations from the first treatment day prior to ICAGD (left) and after ICAGD treatment (right). The Total Body Region Deviations improved considerably after this subject’s occlusion was measurably modified. Improved FHP can be observed pre (left) to post ICAGD (right), that reduced perceived head weight by 54.2%. This subject’s Total Body Region Deviations also improved after ICAGD.
Figure 5 shows the same treated subject’s MatScan Sway data from the first treatment day prior to ICAGD (left), and after ICAGD treatment (right). This subject’s Sway parameters all improved after ICAGD. The yellow arrow points to the reduced sway, recorded post ICAGD. The reduced Sway Area indicates better balance, with increased and centered basal support, both of which are critical in postural stabilization.36
Discussion
Posture’s influence of the Stomatognathic system has been studied, reviewed, and discussed in the literature. A 2020 systematic review found that 67% of the included articles showed a relationship between occlusion and posture exists, while 33% did not.37 It is important to remember that the lack of a significant finding in any study is only evidence supporting a possible absence, not a definitive proof of absence. The findings of this study support and corroborate the Solano et al. systemic review, in that a relationship was found between occlusion and posture in the treated subjects.36This study’s postural sway and forward head posture improvements were also consistent with an observational study (no corrective therapy was administered) by Moustafa et al,11 who found that subjects with FHP had greater sway, and were less stable than a group of matched controls who had less sway and were more stable. In this study, the occlusion was measured and then corrected with ICAGD, while pre and post therapy observational posture measurements were recorded. In the treated subjects following precise and measured occlusal corrections, Sway was reduced and FHP improved. It was also observed that the subjects that had a greater forward head posture had a higher reduction of perceived head weight reduction following DTR.
Of note is that this is the first study to use computer-guided occlusal refinements (ICAGD/DTR), and to examine resultant changes in postural sway and forward head posture. ICAGD is performed in the Maximum Intercuspal Position (MIP), to change bite force distribution and excursive contact timing durations. Working in MIP isolates the occlusal changes from Vertical Dimension alterations and TM joint positional changes that employing a splint induces. This study found that the detected postural improvements resulted from measured occlusal morphologic alterations, and not from VDO and TM joint position alterations.
Primary factors that influence posture are whether one’s eyes are open or closed, and if foot placement changes. Trigeminal inputs are primary as well, because podal posture and spinal alignment can be negatively influenced with misdirected and excessive occlusal contacts.17
Postural control in the static stance is under multiple muscular control strategies. The A-P balance is derived from ankle (plantar/dorsiflexor) control, whereas R/L balance is under hip (abductor/adductor) control.36 The reduction of A-P sway in the control group may be explained by the potential ability of a test subject to reduce entropy with their postural control, by focusing increased attention in their second (same-day) test session.38
Changes in Sway Parameters after modifying trigeminal inputs that affect postural control may be explained through the Inverted Pendulum Model.38 Altering environmental conditions by increasing compliance or decreasing support surface size, combined with any patient sensorimotor impairment, may affect the body’s Virtual Inverted Pendulum (VIP), where the feet act as a pivot that without constant small muscular adjustments, the body would fall over. An unstable VIP can force the brain to carry out massive bodily recruitments to regain stability. This can be seen with a hip strategy that directly equilibrates the Center of Mass (COM) with respect to the Center of Pressure (COP).38
It has been demonstrated that increased maximum bite force generated during forcefully clenching into MIP results from the therapeutic effect of ICAGD.39 An improved ability to clench facilitates soleus reflexes, thereby influencing the stability of postural stance.40
An imbalance between the bilateral masticatory muscles has been shown to antagonistically act on cervical spine displacement, conferring there is compensatory postural control.41 DTR intervention rebalances the forces of occlusion and synchronizes the muscles of mastication, which reduces compensatory stress placed on the cervical spine, improving neck realignment and postural stabilization of the whole body. The FHP and Sway reductions seen in this study are the direct result of this type of cervical spine response to DTR therapy.
Of importance is the periodontal ligament afferents can distinguish the direction forces are applied to teeth,42 and provide afferent instructions to the central nervous system (CNS), which directs masticatory muscles and the swallowing musculature.43 Additionally, tooth pulp and PDL afferent nerve fibers travel directly to the Reticular Formation, which is major brain center that controls swallowing, sleep, breathing, posture and wakefulness. Although the high complexity of its neurophysiological connections is not completely understood, the trigeminal mesencephalic nucleus within the CNS is a primary afferent neuron with extensive central connections that are subject to polysynaptic modulation, suggesting that it has a complex role far beyond that of producing the jaw-closing reflex.44
Evidence also points to other occlusal controls that influence functions separately from the periodontal ligament. Mirales et al. have studied canine guidance in edentulous denture wearers and noticed changes in muscle activity compared to a bilaterally balanced denture occlusal scheme. Bilateral balance is an occlusal scheme that is biomechanically similar to the dentate state of an untreated DTR patient who has long Disclusion Time from bilateral interferences. However, being fully edentulous negates all possible input from the periodontal mechanoreceptors, thus mucosal, muscular and TM joint receptors must be involved with the muscle activity response to canine guided dentures. The authors postulated that a displaced condylar position would provide the missing PDL afference, via a Temporomandibular Joint receptor connected to the motor neurons of the muscles of mastication.45 The inclusion of canine guidance in denture wearers has been linked to improved mastication.46 Canine guidance combined with short Disclusion Time after ICAGD, has been shown to statistically improve human chewing in dysfunctional TMD patients, who (like denture wearers) chewed weakly, slowly, with increased variability and ineffectively before undergoing ICAGD.2
A published Case Report17 about a periodontally hopeless patient, who underwent full mouth extractions, illustrated the neurologic posture control that PDL fibers have on human body stability. When anesthetized in both jaws for the extractions, the patient’s posture worsened, but re-stabilized after immediate dentures established an occlusion, and the anesthesia was metabolized. Interestingly, at the controlled follow up appointment, computer-guided occlusal refinements that redistributed imbalanced forces and shortened closure and excursive timing durations, led to further posture stabilization.17
Occlusion’s importance on patient well-being cannot be overemphasized. Proper chewing function and proper body posture and stability both depend on a well-functioning occlusal scheme. The human body is not a collection of independent systems, but to the contrary, it is a synergetic ensemble of interactive systems with many coordinated functions, that are subconsciously performed in unison.
Obviously, the whole-body effects of postural control and how it changes is incredibly complex. A 2011 systematic review stated, “…the current evidence does not support the usefulness of Posturography as a diagnostic aid in dentistry.”47 In this posture-occlusal adjustment review’s findings they revealed that most of the treated subjects had improved forward head posture. It would appear the previous authors arrived at an incorrect conclusion, even though 2/3rds of the studies they reviewed did find at least a weak correlation. This was also partly due to only reviewing studies that did not biometrically measure both the occlusion and the posture.
Some interesting posture improvements that were seen here amongst the treated subjects but were not statistically evaluated, involved pre to post ICAGD changes in shoulder alignment (Figure 6). Frontally, the left and right shoulder heights frequently became more similar after ICAGD, which was an unanticipated outcome.
In some patients as time evolved, the improvements of decreased FHP were observed beyond those seen directly after subjects underwent ICAGD (Figures 7 & 8). Figure 7 shows the day 1 pre-treatment (left image) posture to post ICAGD FHP immediate improvement (right image). The subject’s right ear aligned closer to, but still slightly forward of the body’s side-view vertical axis. Figure 8 compares the pre-ICAGD posture (left image) to the posture after 6 months’ time had passed since Day 1 of occlusal treatment (right image). Note the subject’s right ear after 6 months is almost exactly aligned with the body’s side-view vertical axis. This ongoing posture improvement occurred concurrently with the patient experiencing minor revisions to her occlusion over time, after visit 1 ICAGD.
Limitations
The apparent added weight of forward head posture is estimated rather than measured, which makes small differences suspect to errors in the estimates. However, consistent large differences are likely reliable. The apparent significant change in the AP Exc of the control group (Table 5) is also subject to question. The Wilcoxon Signed-Rank test may be more sensitive to within-subject change than the resolution of the estimate of AP exc. The mean change was very small.
Conclusions
A strong relationship was found between occlusion and posture, illustrated in the treated subjects’ pre to post DTR via ICAGD occlusal adjustment improved postural Sway and reduced FHP, which was not seen in the control subjects. There are patient consequences and benefits when changing the occlusal morphology of teeth. But it is important to note that all occlusal adjustments are not the same, rendering meaningless the widely advocated blanket statements that neither “TMD or occlusion is related to posture”. Digitally measured occlusal adjustments, made specifically to bite force imbalances and prolonged Disclusion Times, that are performed under very precise and measured outcome tolerances, optimize a patient’s stomatognathic neurology that plays a primary role in both Postural Sway and Forward Head Posture. In addition to performing FHP research, new occlusal therapy projects should be conducted under strict DTR parameter control that involve the shoulders, hips, knees, and ribcage. Furthermore, gait analysis and fall risk should also be objectively studied by combining digital occlusion with biometric posture technology.
Disclosure Statement
The authors received no financial support for this research, or for its authorship or its publication.
Conflict of Interest Statement
The authors reported no conflicts of interest.
_before_composite_application_to_the_maxillary_first_right_molar_.jpeg)
_before_composite_application_to_the_maxillary_first_mol.jpeg)

_and_after_i.jpg)

__the_patient_s_right_shoulder_is_higher_than_her_left._post_icagd_(ri.jpg)
_to_post_icagd_fhp_improvements_(right)._directly_after_the_occlusal_adjus.jpg)
_to_after_6_months_had_passed_from_day_1_.jpg)
_before_composite_application_to_the_maxillary_first_right_molar_.jpeg)
_before_composite_application_to_the_maxillary_first_mol.jpeg)
_and_after_i.jpg)
__the_patient_s_right_shoulder_is_higher_than_her_left._post_icagd_(ri.jpg)
_to_post_icagd_fhp_improvements_(right)._directly_after_the_occlusal_adjus.jpg)
_to_after_6_months_had_passed_from_day_1_.jpg)