Introduction (from Part I)
Temporomandibular Disorders (TMDs) are a category of at least 40 distinct conditions negatively affecting the function of the stomatognathic system.1 Many TMD conditions include internal derangements of the articulating disc within the temporomandibular joint that is often followed by degenerative changes in the joint.2,3 The degenerative progression is most strongly related to disc displacement without reduction.4 Some studies have found that TMDs are likely to result from the partial or complete loss of molar dentition causing mainly muscular symptoms (orofacial pain).5–7 Others have found that occlusal interferences to function can precipitate TMDs,8–11 while divergent studies have been unable to find any etiologic relationship with occlusal variables,12 especially within short-term and pilot studies.13 A separate skeletal structural issue related to the masticatory system is Angle’s occlusal classifications. There is evidence that Class II occlusal arrangements have a greater propensity toward developing substantial TMDs symptoms, but Class II and other skeletal problems can also result from the structural consequence of TMJ damage.14–16
Congenital conditions such a cleft lip and cleft palate have been shown to reduce the quality of life and masticatory function even after treatment.17 Ehlers-Danlos syndrome is another genetic disorder that increases the propensity toward developing TMDs.18 One recent study concluded that single-nucleotide polymorphisms can aid or abet the development of TMDs after orthognathic surgery.19 Abnormal growth and development have also been identified as contributors to TMDs conditions. Bacterial infections have been found to be significantly more prevalent in TMDs patients than in healthy subjects.20–23
Psychoneuroimmunology has theorized that emotional stress can be either an etiologic factor or an exacerbating factor in precipitating or perpetuating TMD and chronic orofacial painful conditions.24–26 Somatization, recently renamed as Somatic Symptom Disorder (SSD), has been proposed as a primary etiology of at least some TMDs and orofacial pains.27 The Research Diagnostic Criteria (RDC/TMD),28 in Axis II, has recommended the Beck Depression Inventory-II to measure depression and the subscale of the SCL-90 to evaluate somatization.29 However, it is common knowledge that SSD cannot be distinguished just by symptoms from underlying physical conditions/diseases because they simply share the same symptoms. It was stated in the RDC/TMD that the SCL-90 does not measure somatization. Of course, psychiatry understands very well that all possible physical sources of symptomology must be discounted before testing for SSD is likely to be efficacious.
The Patient Health Questionnaire-15 (PHQ-15), validated by testing a large normal population, is a fifteen-question anamnestic instrument used by many psychiatrists and psychologists to evaluate SSD in the absence of a definite indication of any physical etiology.30 See Figure 1.
Each question is supplied with three possible answers; 1) not bothered at all, 2) bothered a little, or 3) bothered a lot (during the past 7 days). The totaled score ranges from 0 to a maximum of 30. Normative scores across the population are generally less than 5 and increase gradually with age. Moderate SSD is indicated by scores from 10 to 14, while a score of 15 indicates a percentile rank between 92.8 and 99.7.30 Higher scores = higher probability. See Figure 2.
With so many factors potentially contributing to TMDs it is not surprising that controversy has been the most common overall result of TMDs research. A previous study that utilized the Beck Depression Inventory-II, compared depression scores from TMDs subjects pre to post successful physical treatment. While most of the subjects had exhibited moderate to severe depression pre-treatment, successful physical treatment reduced all of their levels to within normal limits, removing depression by itself as a potential etiologic factor for the group.31
Objectives
The objectives of this report were 1) To compare the changes in the PHQ-15 scores to the changes in the masticatory function as indicated by EMG and EGN data and 2) to compare the progression of pain intensity, frequency of symptoms and functional restriction scores to the concomitant progression of masticatory function. The Null hypothesis = No correlation between the PHQ-15 scores or any of the symptom mean scores and the masticatory motion and muscle activity parameters.
Methods
For this study six highly experienced private practices specializing in the treatment of TMDs patients were
recruited from four countries (U.S.A., Mexico, Brazil and India). Two of the practices (PT & BS) focused specifically on treatment of TMDs patients without serious TMJ involvement, which could also be termed Orofacial Pain patients with a preponderance of orofacial, painful, muscular symptoms and an absence of TMJ pain. Their treatments were limited to adjusting the occlusion using a well-established protocol for the T-Scan (Tekscan, Inc. South Boston, MA USA) linked to the BioEMG-III (Bioresearch Associates, Inc. Milwaukee WI USA) commonly referred to as Immediate Complete Anterior Guidance Development (ICAGD) or Disclusion Time Reduction (DTR).32–39
The other four practices were focused on arthrogenous TMD patients, most of whom had some stage of Internal Derangements of the TMJ from relatively acute to end-stage chronic conditions. Their treatment methods were varied and included the individualized application of ULF-TENS, a mixture of orthotic appliances, NSAIDs, exercises and selected orthodontic and/or prosthodontic restorative treatments for the final restoration of normal function.40–44 These four private practices were thoroughly dissimilar, geographically separated and not linked in any manner, with distinct treatment philosophies and methods. This was intentional to include a variety of treatment methods from a non-uniform group of practitioners.
To document the symptom levels prior to treatment each practice agreed to record an anamnestic survey of each patient’s Pain Intensity, Symptom Frequency and their Functional Restrictions. See Figures 3 to 5. The questions used were taken from popular symptom surveys (e. g. RDC/TMD). After each patient had signed informed consent and agreed to treatment, they were also given the PHQ-15 instrument to respond to. All four of these anamnestic instruments were re-utilized approximately 3 weeks after initiation of treatment and at 3 to 4 months post-treatment at a follow-up appointment.
All patients were recorded pre-treatment, post-treatment and at follow-up with Joint Vibration Analysis (JVA) to evaluate TMJ function.45–59 At the same appointments masticatory function was also assessed with combined electrognathography (EGN) and electromyography (EMG) recordings of gum chewing.60–71 This was done to evaluate; 1) the function of the TMJ and 2) the quality of mastication of a soft bolus (gum) using BioPAK software (BioResearch Associates, Inc. Milwaukee, WI USA). The recordings were repeated at each appointment and at the follow-up appointments. The analysis of the masticatory function data is reported in this Part III.
Student’s Paired t test was applied to the measured intra-patient EGN and EMG data, making each subject his or her own control. Consequently, no separate control group was enlisted because the purpose was simply to correlate the masticatory function data with the symptom levels and PHQ-15 scores. Wilcoxon Signed Rank test was applied to the survey data (Pain, Symptom Frequency, Functional Restriction and PHQ-15 scores) to detect significant improvements. In this third report, Spearman Correlation was used to compare the EMG and EGN data to the PHQ-15 scores, the Pain scores, the Frequency of Symptoms scores and Functional restriction reports. Alpha = 0.05.
A total of 82 patients participated, 61 females and 21 males at a ratio of 2.9:1. The mean age was 43.4 (+/- 17.2) years with a range from 14 to 76 years and a median of 42. While the age distribution was not a normal one, it does represent a range of likely candidates. This is a little older group than many previous TMD studies, which have had their mean ages in the mid to late 30s. Patients were selected sequentially as they agreed to participate. Although not a random process it fairly represents the TMD population both for patients with TMJ involvement (43) and those without TMJ involvement (39). An IRB Exemption for this study # BIRB/100Z/2019 was received.
Results
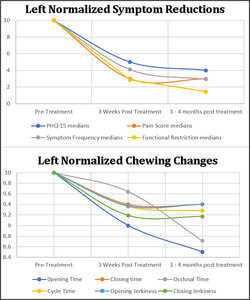
Significant improvements were observed in all symptom categories. Total pain intensity scores were extracted from the Symptom Pain Scale levels that were reported pre-treatment, 3 weeks post treatment and again at 3 – 4 months post treatment. See Table 1.
In addition to their recording of pain scores, each patient was required to record the frequency of their symptoms, which was tracked prior to and throughout treatment. See Table 2.
The group’s Functional Restriction median scores were significantly reduced by the treatments. See Table 3.
A dramatic reduction in PHQ-15 scores occurred post treatment. See Table 4.
A comparison between DTR and orthotic treatments showed no significant difference in scores prior to treatment but a significant difference post treatment. See Table 5.
A comparison of the results of treatment between the two groups manifesting either; 1) occluso-muscular or 2) TMJ internal derangement symptoms is shown in Table 5. Those cases that had primary occluso-muscle symptoms and no substantial involvement of the TMJ had their Disclusion Times Reduced (DTR) with Immediate Complete Anterior Guidance Development (ICAGD).31–34 The TMD subjects with substantial TMJ involvement (Internal Derangements) were treated with orthotics, TENS, NSAIDs, exercises and other commonly applied methods. Most of these primarily arthogenous patients also had secondary muscular pain complaints that were significantly reduced by treatment as well. It can be seen from this comparison that the orofacial pain patients responded to a greater extent and more quickly within 3 weeks and at the 3 to 4 months timepoint.
EGN & EMG Data
(See appendix for more details)
EGN (motion) & EMG (muscle activity) were recorded bilaterally simultaneously and analyzed together. Five of ten parameters from the analysis of the left side EGN data were found to be significantly improved towards normal values at 3 weeks post treatment. See Appendix for normal values. This increased to eight of ten parameters by 4 months after the start of treatment. Tables 6 & 7.
The vertical dimension was determined by the size of the bolus and was stable as expected. The significant decrease in the durations of opening, closing, the occlusal times and the cycle times approached normal values (See appendix for normal values). Note: Five subjects did not record chewing at three weeks and eight were missed at follow-up. For the left side, five additional parameters were analyzed. See Table 7.
The A/P Turning Point is the antero-posterior position of the most open point in the chewing cycle. Although the vertical dimension of the Turning Point did not change, the A/P dimension increased significantly. The opening and closing velocities both increased significantly by follow-up, one indication of increased confidence. The closing jerkiness of chewing decreased significantly (smoother motion) and the opening jerkiness showed a similar trend.
The Opening Time and the Occlusal Time changed the most between the 3 weeks and the 3 – 4 months. Figure 6.
Significant decreases were found in the timing of the opening, closing, occlusal and cycle times during right-side chewing. See Table 8. Like the left side chewing, no change was recorded in the vertical dimension of the right-side chewing.
Five additional right-sided chewing parameters were significantly changed in a very similar way to the left-sided chewing with increased A/P Turning Point, increased opening and closing velocities and reduced jerkiness. See Table 9. Figure 7 graphically relates the reduction in symptoms to the changes in the movement parameters.
Correlations were found using the Spearman correlation coefficient as a suitable non-parametric statistic. Figure 8.
A significant strong correlation (0.767 – p = 0.0159) was found between the progression of the symptoms and the progression of the changes in the A/P Turning Point, the opening Jerkiness and the closing Jerkiness for left-side chewing. The A/P Turning Point progression was reversed because it was determined to be inversely proportional rather than directly proportional like the jerkiness. A very similar correlation was also found between the symptoms and the right-side chewing parameters of reverse A/P and jerkiness (rs = 0.728, p = 0.02615). See Figure 9.
While the A/P Turning Point is a function of the opening and closing chewing pathways, the jerkiness is directly related to the smoothness of the chewing function. For additional explanation of the Turning Point and how the jerkiness is measured see the appendix.
EMG Chewing Activity
Muscle activity was recorded and evaluated during left and right-side chewing. Five parameters were calculated for each subject.
-
Mean Area under the rectified average activity
-
Coefficient of Variation (the standard deviation of the Mean Area divided by the mean)
-
Peak Amplitude of the averaged chewing burst
-
Time to Peak (from onset of the chewing cycle to the peak of the averaged activity)
-
Peak to Occlusion (peak activity to end of closure)
The EMG activities in Tables 10 and 11 were recorded along with the EGN movement data, which was used to segment the cycles for averaging. The averaged cycles from each subject were then used to create the group means for each muscle. The significance was calculated between pre and post treatment using Student’s Paired t test after checking all of the data for sufficient normality.
Discussion
One important stand out general finding of this study in agreement with previous work was that both the physical and emotional responses to treatment in this group required several months’ time to achieve the maximum effects.31,36–38 This was seen for the PHQ-15 scores, the reported symptoms, the chewing motions and the muscle activity, even for those patients that experienced an initial rapid reduction in symptoms.
Spearman’s Correlation Coefficient is non-parametric and appropriate for survey data because it does not require the assumptions of the Pearson correlation. Its formula is:
p=1−6n∑k=0d2 n(n2 −1)
p = Spearman’s rank correlation coefficient
di = difference between the two ranks of each observation
n = number of observations
EGN Chewing Motions
Spearman’s Correlation Coefficient was calculated for the relationship between the Pain scores, the Frequency of Symptoms scores, the Functional Restrictions scores and the PHQ-15 scores Vs the EGN Opening and Closing Times, the Opening Jerkiness and the Closing Jerkiness. See Figures 8 & 9.
rs = 0.7164 for the left chewing, 0.8094 for right chewing
These were relatively strong correlations.
The mean and median PHQ-15 scores of the group were reduced significantly as treatment was provided and they continued to significantly reduce four months later at the follow-up appointments along with the changes in the EMG and EGN parameters. From the graphs in Figures 6 & 7 it appears that neither the PHQ-15 scores nor some of the EGN parameters have reached their absolute minimums at four months after the onset of treatment for all subjects. Additional time may be needed for some in this group to achieve maximum medical improvement.
To graph five of the EMG parameters together, the post treatment values were normalized to pre-treatment values of 1.0. These graphs show the changes as either increasing or decreasing over time. See Figures 10 & 11.
EMG Chewing Activity
Note in Table 10 that the Mean Area (the total of the left side EMG activity) and the Mean Peak Amplitude were increased substantially in both over the 4-month interval. This suggests an increase in the forcefulness of mastication. Simultaneously, the timing durations and the variability were reduced (faster mastication with more consistent muscle activity). In this group the mean time from Peak EMG to the End of Closure (Occlusion) was not negative pre-treatment, but for very dysfunctional TMD patients it often is, indicating a hesitancy to close forcefully into occlusion.
The right-sided mastication produced similar changes in the EMG activity during mastication. See Table 11. The one difference between left and right mastication was that the time from the Mean Peak of the EMG Activity to Occlusion increased during right-sided chewing. This difference was due to an earlier peaking of the muscle activity. The increase in right-sided chewing rate can be seen in Table 8 as the cycle time was reduced from a pre-treatment mean of 895 milliseconds to a post treatment mean of 808 milliseconds, which is closer to a mean normal value. The increase in the time from the Peak to the Occlusion from a pre-treatment value of 32.4 milliseconds to a post treatment value of 72.3 milliseconds replicates a more normal value and indicates greater confidence in chewing, whereas the 32.4 milliseconds value was abnormally small. See the appendix for normal values.
A significant change was recorded in the mean position of the antero-posterior Turning Point. This is the most open point in space where the end of opening transitions into the beginning of closure. The mean amount of the change was greater with right-side chewing than with left side chewing, which suggests the right-sided function may have been more restricted pre-treatment. In the patients treated occlusally it is possible that their muscle action was freer after removal of the occlusal restrictions. In those patients with joint involvement, the gradual healing of those TMJ structures may have ultimately allowed freer motion post treatment.
TMD and Orofacial pains that are associated with occluso-muscular TMD symptoms have previously been shown to be significantly reduced up to five years and longer after ICAGD treatment.72,73 Some reduction in symptomology can occur instantaneously, but to reach maximum medical improvement (MMI) requires some extended time-period for full recovery. Treatment by appliance also usually requires six to twelve months to achieve complete MMI.74
This time is required for healing and tissue adaptation, especially in avascular tissues as in those parts of the TMJ with slow metabolite infusion.75 A period of up to six months or more to successfully reduce painful symptoms in TMJ involved (arthrogenous) cases has been commonly observed. This suggests that attempting to diagnose SSD within TMD patients prior to the completion of physical treatment and recovery could produce a false positive SSD diagnosis. Pain is purely subjective, and the etiology can only be determined if the pain can be relieved by some controlled means. Removing the pain pharmacologically does not reveal the etiology but masks it. Based upon the results of this investigation we reject our null hypothesis of no correlation between the PHQ-15 scores or any of the symptom median scores in relation to the masticatory motion and muscle activity parameters.
The Symptom Frequency scores improved significantly after treatment and continued to improve significantly even up to the follow-up appointment three to four months later. This supports the concept that the group responded to all the treatments by reducing the frequency of their symptoms significantly, but symptom reduction is not instantaneous. Three to four months of physical treatments and gradual recovery were required before the symptom frequencies subsided, which is a common finding in many TMD treatment studies.76,77
The goal of evaluating functional restrictions is to reveal whether the subject is experiencing difficulty chewing, swallowing, has excessive tooth sensitivity or has been avoiding any tough foods. Although the term functional restriction is often applied just to a limited range of motion, it would be a more appropriate indicator if applied to masticatory capacity. When capacity is only based upon the subjective reporting from the patient, it is a weaker measure than when an objective method is used.78 Masticatory function as reported here is an objective measurement of the degree of normality. Although one does not need to function exactly as the mean normal parameters, they do represent reasonable targets for the purpose of assessing improvement.
Comparing one obvious difference between the 2 methods of treatment, the ICAGD is focused on the occlusion, specifically occlusal interferences to masticatory function. The orthotic approach is usually focused on arthrogenous conditions and the correction of a existing maxillo-mandibular mal-relationship, whether due to TMJ internal derangements, any developmental abnormality such as crossbite, orofacial trauma or simply missing molars. The occlusion is more readily corrected by ICAGD when no serious TMJ condition is present but can sometimes also improve an arthrogenous TMD patient’s condition enough to reduce symptoms to a tolerable level. There does not appear to be a downside to ICAGD when it is done carefully and with expertise.
Since muscular symptoms can also result from a maxillo-mandibular mal-relationship, an orthotic can often reduce muscular symptoms as well, especially if existing internal derangements are well adapted. However, the success of an orthotic may need to be maintained with some form of permanent correction (prosthodontic or orthodontic) if a gradual “weaning” of the patient from the appliance does not suffice. Under some economic circumstances a durable “permanent” orthotic appliance may alternatively be prescribed.
The PHQ-15 median score of this group of TMD subjects dropped from 10 (medium SSD) pre-treatment to 4 (within normal limits) after physical treatments. Within this group 46 had pre-treatment PHQ-15 scores > 10. A premature attempt to establish an SSD diagnosis using PHQ-15 would have misclassified 58 % of the group as medium level or higher SSD. At the three to four months timepoint 15 % of the group had a PHQ-15 score > 10 (median score 11). The fact that even these resistant cases had significantly reduced their scores from a median of 20 to a median of 11 (p = 0.0116) suggests that they had physical TMD etiologies that responded positively to their physical treatments. Their mastication parameters improved in parallel with the changes in symptoms, with the changes in the PHQ-15 scores and were highly correlated. See Figures 7 and 8.
While it is plausible that the more resistant patients may also have some emotional aspect to their TMD, more time would be needed to establish that within this group. At 6 months or even at 12 months their scores may also fall to within normal limits. Those with PHQ-15 scores that remained above normal at 3 – 4 months also still had painful symptom scores and perhaps additional etiologies.
Limitations
While the ICAGD treatments are standardized and have been successfully reported from different practitioners in previous studies,35,37–39 the other four practices providing orthotic-based treatments were quite diverse and the patient populations included TMJ internal derangements that were more complicated to treat. Since this study focused on treatment outcomes with the subjects only being compared to themselves, no control or placebo group was included. This was also the design because it can be very difficult to maintain active placebo treatments for several months for TMD subjects that are in pain.
Conclusions
The pre-treatment PHQ-15 median score of the group was significantly reduced after physical treatments. Thus, it could have been considered a false positive indication of SSD prior to any physical treatment. Also, the PHQ-15 scores continued to significantly reduce at 3 – 4 months, even well after the end of physical treatment. Correlations were found between the significant improvements in the left and right-sided masticatory timing, motion and muscle function with respect to the PHQ-15 scores. This result supports primarily a physical rather than an emotional etiology for this group’s TMDs. Consequently, the null hypothesis was rejected.
Clinical Significance
The data in this report supports the theory that the diversity of TMD symptoms can best be explained as predominantly due to physical conditions and only rarely can they be attributed purely to psychosocial etiology. Along with reductions in symptomology and an improved emotional status, this measured mastication data study suggests that corrective physical treatments can also be effective at improving masticatory function, even in moderately affected cases. Oral diseases and disorders routinely have physical etiologies that need treatment prior to testing for somatization, which is the standard of care approach recommended by Psychiatry.79
Declaration of conflicts statement
John Radke is the Chairman of the Board of BioResearch Associates, Inc. No other author reported any potential conflict of interest.
Funding Statement
No funding of any kind was received in support of this research activity.










_shows_the_cycle_shape_and_the_turning_point_at_the_m.jpg)

_of_an_angle_s_class_i_control_subject_exhibiting_the_normal_h.jpg)














_shows_the_cycle_shape_and_the_turning_point_at_the_m.jpg)

_of_an_angle_s_class_i_control_subject_exhibiting_the_normal_h.jpg)


