Introduction
A subset of patients diagnosed with Temporomandibular Disorders (TMD) that exhibit primarily painful muscular symptoms often accompanied with complaints related to their teeth and gingival tissues, is sometimes referred to generically as Occluso-muscular TMD or Orofacial Pain.1 These labels apply to symptomatic TMD patients do not have substantial complaints related to their Temporomandibular Joints. Orofacial pain has been further delineated to include neuropathic pain2 and fibromyalgia.3
The T-Scan (Tekscan, Inc. South Boston, MA USA) and BioEMG III (Bioresearch Associates, Inc. Milwaukee, WI USA) guided occlusal adjustment procedure that reduces functionally-interfering posterior occlusal contacts of long duration is known as Immediate Complete Anterior Guidance Development (ICAGD).4 It is also referred to as “Disclusion Time Reduction (DTR)” because a Long Disclusion Time (≥ 0.5 seconds)5,6 in lateral excursion is the key variable describing the time-duration that functional posterior occlusal interferences frictionally engage during an excursion. See Figure 1. That duration if lengthy, creates high levels of excursive functional muscle activity, that weakens the masticatory and swallowing muscles with lactic acid ischemia, to cause many common muscular TMD symptoms. Removing prolonged functional posterior excursive interferences with the T-Scan 10/BioEMG III guiding ICAGD, has previously been shown to statistically reduce the Disclusion Times and the high levels of masticatory muscle activity occurring during the excursion. This in turn arrests ongoing lactic acid production to oxygenate and restore muscle capacity, which produces significant reductions in both chronic physical and emotional symptoms.5–15
To demonstrate the physiologic effects of DTR, masticatory functional gum-chewing motions were recorded with the magnet-based incisor-point tracker JT-3D and the BioEMG III (BioResearch Associates, Inc. Milwaukee, WI USA). See Figure 2a. These 15-20 sequentially recorded gum chewing cycles. See Figure 2b. after software calculation, generated an individual subject’s Average Chewing Pattern (ACP).16 See Figure 2c.
Certain aspects of the velocity of gum-chewing can indicate present masticatory dysfunction. The maximum closing velocity is reduced when the subject is hesitant, required to avoid occlusal interferences, or has a skeletally misaligned centric occlusion position. Even with a more resistant bolus, the typical asymptomatic subject produces a peak closing velocity ≥ 100 mm/second. When plotted next to each other, obvious visible differences between a dysfunctional subject’s velocity (Figure 3; left pane) and an asymptomatic control subject’s velocity become readily apparent. See Figure 3 - right pane.
From the motion recordings the velocity, acceleration, and the jerk derivatives can also be calculated.17 The jerk function is simply the 3rd derivative of motion calculated to describe the rate change of acceleration (Jerk = d3x/dt3).18 When chewing motion includes frequent changes between acceleration and deceleration, it can be described as “jerky” or “not smooth.” The jerk function therefore characterizes the lack of smoothness within the masticatory movements.19,20 Importantly, the introduction of occlusal interferences can increase the jerk-cost, reducing smoothness.21
Masticatory smoothness can be evaluated by counting the inflection points in the acceleration waveform, which indicate the transitions between chewing acceleration and deceleration across time. They are particularly relevant during the closing stroke of masticatory function. The inflection points are where the waveform changes from concave downward to concave upward, or vice versa. See Figure 4. A perfectly smooth chewing cycle demonstrates only 2 inflection points during closing;
-
One transition from opening deceleration to closing acceleration
-
One transition from closing acceleration to closing deceleration
Conveniently, the Jerk function peaks at each acceleration inflection point.
Counting the jerk function peaks (which are visually more obvious than the acceleration waveform inflection points), allows for calculating the mean number of jerk function peaks per close, over a series of masticatory cycles. Softened gum has low resistance, which minimizes any disruptive bolus effects during chewing, such that any lack of chewing smoothness detected would not be caused by the bolus, but instead from masticatory system dysfunction. Alternatively, a brittle-consistency bolus that can fracture from resistance to being crushed, will also disrupt the smoothness of the closing waveform. See Figure 5.
In asymptomatic control subjects, while muscle activity levels change from cycle to cycle as required to manipulate the bolus, the overall chewing motions tend to remain consistently smooth, absent of dysfunctional characteristics. The data from the asymptomatic control patient in Figure 6 is fast and smooth without hesitancy, even though the muscle activity changed for every cycle, as is required to manipulate the bolus. Although the bolus is manipulated and masticated with different levels of activity from each muscle during each closure, the muscular coordination is so precise that it produces smooth overall function.
In contrast, the jerk function from a dysfunctional subject often includes many small peaks, making the visual counting of peaks difficult. See Figure 7. However, that is simplified by using electrognathographic software analysis tools to count the peaks. Note that in Figure 7 the EMG activity is less variable, slower, and less intense compared to Figure 6. Instead of the muscle activity instantaneously adjusting to the bolus as needed, the less variable muscle activity either avoids premature contacts in the occlusion, or accommodates motion limitations imposed by a damaged Temporomandibular Joint.
Objective
To evaluate the effect of Disclusion Time Reduction on the maximum closing velocity and smoothness of gum chewing in dysfunctional TMD patients. The Null hypothesis: No significant changes occur in the mean maximum closing velocity or the mean number of jerk function peaks from subjects after undergoing ICAGD.
Methods
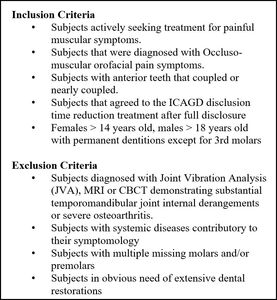
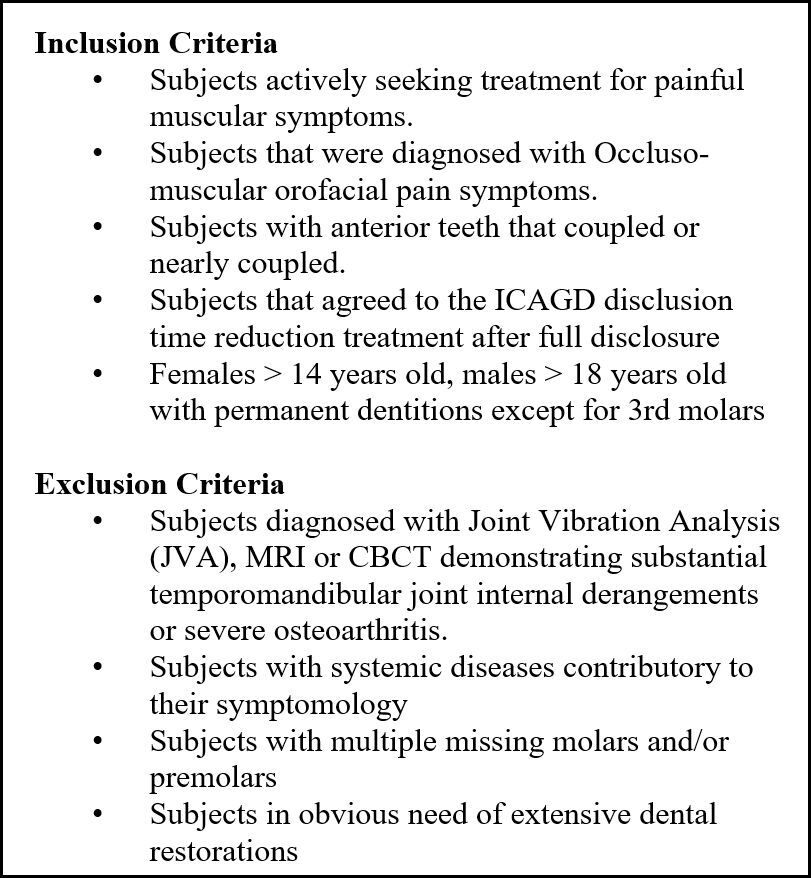
The patient records of 34 TMD patients (23 females, 11 males; mean age = 34.9 +/14.76 years) with primary muscular symptoms that actively sought treatment for their painful muscular symptoms, were reviewed for the relevant information regarding their ongoing symptom history and treatments they previously underwent that had not resolved their chronic pain conditions. Subjects with severe Temporomandibular Joint dysfunction were excluded after JVA analysis. Figure 8.
Pretreatment gum-chewing EGN incisor-point motion records with EMG data sets of the 34 muscularly dysfunctional OMD patients, were reviewed. The included subjects all demonstrated chewing fatigue, chewing pain, or chewing weakness, and experienced ongoing head, neck and facial pain, headaches around the eyes, midface and temples and jaw tension. Subjects reported previous unsuccessful splint use, chronic pain medication ingestion, and/or mildly painful Temporomandibular Joints. All included subjects were required to have anterior teeth that coupled or nearly coupled.
The records included left and right directed gum chewing sequences of at least 15 cycles. Surface electrodes were applied to the bilateral anterior temporalis and masseter muscles and a magnet placed on the mandibular incisors in the labial vestibule below contact with the maxillary incisal edges, which simultaneously captured the incisor-point motions from the JT-3D and muscle activity from the BioEMG III. The motion data were used to segment the sequences into individual cycles, which were then averaged to produce the Average Chewing Pattern (ACP) of motion, and the Average Chewing Cycle (ACC) of muscle activity. The data files were analyzed with the BioPAK™ program (Bioresearch Associates, Inc. Milwaukee, WI USA) by first segmenting each sequence into individual cycles and then calculating the ACP, which was then used to calculate the ACC. This process also reveals the subject’s mean maximum closing velocity and the mean number of inflection points within the closing portion of the acceleration waveform as peaks in the Jerk function (see Figures 4 and 5).
The process of Disclusion Time Reduction with the ICAGD coronoplasty has been described previously,14,15 and has the objective of removing posterior occlusal contacts during lateral excursions to very high-precision time duration tolerances. This process is guided by the T-Scan 10 and accomplished in one appointment, but often requires up to three follow-up appointments. The goal of the ICAGD adjustment procedure was to reduce the time required to disclude all posterior teeth in a lateral excursion in less than 0.5 seconds. The endpoint of the adjustment statistically reduces EMG activity levels during the treated lateral excursions.
A gender and age matched control group of asymptomatic subjects (mean age = 32.9 +/- 12.72 years; p < 0.2757), was comprised of 23 females and 11 males that were extracted from a large gum chewing database of asymptomatic subjects that were previously recorded with the JT-3D/BioEMG III technologies using the same gum chewing protocol that was used with these 34 occluso-muscle disorder subjects.22 This previously recorded data from asymptomatic subjects was compared to the 34 occluso-muscle disorder patients prior to, and after each treated subject underwent ICAGD. All treated subjects signed an Informed Consent form and the study protocol was evaluated by the IRB review board, which granted an exemption (BIRB/95Z/2021).
Group mean maximum closing velocities and jerk functions were calculated from each subject’s left and right chewing data prior to undergoing ICAGD treatment (n = 68). First, the Disclusion Times and EMG data were measured. Then the ICAGD coronoplasty was applied to shorten the right and left Disclusion Times by removing as much as was possible, all posterior excursive frictional interfering contacts from the molar and premolar teeth. This was done to very high numerical tolerances that were verified by the post ICAGD T-Scan/BioEMG III synchronization data sets (DT ≤ 0.5 seconds/excursion).4,9,14 The post ICAGD left and right lateral excursive Disclusion Times were measured immediately after ICAGD on Day 1 and 3 months later. Also post ICAGD, the exact same gum chewing recording protocol was repeated to obtain new samples of each subject’s gum chewing function data.
The combined left and right gum-chewing records pre and post ICAGD (34 pre; 34 post) produced 68 mean closing velocities and 68 mean numerical jerk function curves. The group means were then calculated by averaging the 68 individual subject’s mean velocities and mean numbers of acceleration inflection points. The exact same process and identical chewing parameters were calculated from the records of the selected gender and age-matched control asymptomatic subjects, which were compared to the ICAGD treated subjects (Alpha = 0.05). See Table 1.
Statistics
The intra-patient Disclusion Time data and gum chewing closing velocity data underwent the Student’s paired t-test. The comparisons between groups utilized the unpaired Student’s t-test. To analyze the intra-patient jerk function peak counts, the Wilcoxon Signed-Rank Test was used, while the Mann-Whitney U test compared the jerk function peak counts between groups (Alpha < 0.05).
Results
Disclusion Time
The mean Disclusion Times for all but two patients were significantly reduced, for an average reduction of 1.56 seconds, but two remained unchanged. See Table 1. Although the Disclusion Time s of most of the treated patients were dramatically reduced after ICAGD, 25 % of the patients treated could not be reduced to an ideal Disclusion Time less than 0.5 seconds. Although the treated patients did not reach the same degree of smoothness as the asymptomatic control group, all three measured parameters moved significantly in the direction of the control group’s values.
Maximum closing velocity
The mean maximum closing velocity increased significantly after ICAGD (p < 0.00001), approaching that of the control group. Although the treated group mean maximum closing velocity did not equal the mean value of the control group, some of the individuals did reach the control value after treatment (Table 2).
Closing Smoothness
The mean number of jerk function peaks reduced significantly after ICAGD treatment (p < 00001), indicating that the chewing smoothness improved. Although the mean of the treated group did not achieve parity with the mean of the control group, a number of the treated individuals demonstrated closing jerk peak values within the control group mean jerk peak value (Table 2).
Discussion
The results of this follow-on investigation indicate that the chewing jerkiness observed in the treated subjects improved significantly within one week after the subjects’ pre -ICAGD mean prolonged excursive Disclusion Times were shortened to less than 0.5 seconds by ICAGD. For the group as a whole, there were significant reductions in the numbers of acceleration inflection points in both the opening closing portions of the cycles. Also, the increases in the mean closing velocities suggest improved function was obtained from the subjects after undergoing ICAGD (See Table 2). Of note is that 28 % of the treated subjects produced velocities within the 95 % confidence interval of the control mean. These results strongly indicate that within one week following ICAGD, this dysfunctional group’s combined masticatory functions in aggregate changed significantly, improving the ability of the group to chew gum faster and smoother. Importantly, this study’s results directly support the findings of the earlier Average Chewing Pattern (ACP) study23 and an additional follow-on chewing smoothness study.24 The observed Jerk peak improvements mirrored the improvements seen in many ACP parameters.23 And this study’s results support the findings of previously published Disclusion Time Reduction/ICAGD studies, where chewing improvements accompanied the reduction of many chronic muscular OMD symptoms.5–15,23
In a previous study of subjects with verified TMJ internal derangements, it was determined that slow dysfunctional mastication was associated with lower values of the integrated jerk function, while fast dysfunctional mastication was associated with higher averaged Jerk function levels.10 In the present study, since the ICAGD treated group increased their mean maximum closing velocity while reducing the number of Jerk function peaks, smoother masticatory function was achieved. It should be noted that the increased mean maximum velocity and the reduced mean number of Jerk peaks moved the treated dysfunctional subjects towards the values of the control group, indicating that reducing the excursive movements Disclusion Times, improved masticatory function smoothness.17
Changes in the ACP can be visually observed and numerically calculated within the post-ICAGD Average Chewing Pattern (ACP) graphs,23 which illustrate the pre and post-ICAGD ACP of one subject. See Figure 9. With short Disclusion Times bilaterally, the subject’s velocity is markedly increased, their ACP planar shapes (red opening & cyan closing lines) more closely match the control shapes (black lines), and their smoothness is significantly improved (Jerk peaks reduced from 9.8 to 5.3 during closing). The fact that post-ICAGD this subject’s velocity substantially increased while the number of Jerk peaks decreased, supports a more normal overall masticatory function. This was also true for the subject group as a whole, in that the group’s mean closing velocity increased significantly while the mean number of Jerk function peaks significantly decreased. While the objective of changing a patient’s chewing function to perfectly normal could be laudable, it is not realistic. However, measurable improvements towards normal parameters are most often significant to the patient after ICAGD.
To evaluate additional chewing function improvements in the same subject in Figure 9, the Averaged Chewing Cycle (ACC) was calculated from the pre- and post ICAGD recordings. See Figure 10. The Averaged Chewing Cycle pattern of muscle function illustrates how masticatory muscle activity improved after ICAGD. The chewing cycle duration decreased from more than 1.5 seconds/cycle down to 1.0 second/cycle. The averaged coefficient of variation decreased from 0.37 to 0.23, indicating the pattern of muscle contraction was substantially more consistent. The hierarchy of the muscle pattern did not change, but the distribution of muscle activity appeared similar to that of normal control occlusal Class II pattern.
An example of a single subject’s Jerk function improvements can be seen in Figure 11. The number of peaks in the Jerk function were reduced while chewing velocity increased. It is noteworthy that the increased Jerk amplitude post-ICAGD (doubling from 15 pre-ICAGD up to 30 post-ICAGD) indicates this subject chewed with increased velocity and acceleration. During opening, the number of Jerk peaks reduced from 6 to 3. In closing the number of Jerk peaks also were reduced by about half (from 14 to 7).
Limitations
A limitation was that additional treated subjects were added into group of re-analyzed prior ICAGD treated subjects, to increase the subject pool size by 33%. However, unlike the first study that used data from some of this study’s ICAGD treated subjects who were their own controls pre to post-ICAGD, the 34 ICAGD treated subjects in this study were functionally compared to an asymptomatic control group that was age and gender matched.
Conclusion
Within this group of muscularly dysfunctional subjects, shortening the Disclusion Time with the Immediate Complete Anterior Guidance Development (ICAGD) coronoplasty to lessen the time-durations of noxious opposing frictional excursive occlusal contacts, allowed the dysfunctional treated subjects to chew gum faster and smoother, approaching the chewing parameters of asymptomatic normal subjects.
Funding
No Funding was received for this study.
Potential Conflicts of Interest
The 1st author (Robert B. Kerstein, DMD) is a Clinical Consultant for Tekscan, Inc., S. Boston, MA, USA, and receives no compensation for sales of any Tekscan product. The 3rd author (Mr John Radke), is the Chairman of Bioresearch Associates.



_with_the_closing_acceleration_(grey_line)_inflec.jpeg)
_of_this_control_subject_.jpg)


_after_icagd_treatment._the_mean_peak.jpg)





_with_the_closing_acceleration_(grey_line)_inflec.jpeg)
_of_this_control_subject_.jpg)


_after_icagd_treatment._the_mean_peak.jpg)

