INTRODUCTION
The first recognition of what are currently referred to as temporomandibular disorders (TMD) was made by Dr. James B. Costen (b. 1895, d.1962), an otolaryngologist in Saint Louis, MO in 1934.1 Lacking in any identifiable pathology, he observed that some of his fully edentulous patients with symptoms of hearing loss, otalgia, tinnitus, dizziness, headache and burning sensations of the throat, tongue and mouth, were greatly relieved of their symptoms after receiving complete removable dentures.
He referred more than 100 such patients to his dentist friend. After the majority of them experienced great relief, he published in the Annals of Otology, Rhinology & Laryngology, presumably to inform his colleagues that a dentist might be of help with similar patients. He attributed the etiology for the symptoms directly to dysfunction in the TMJ and malocclusion. This has been thoroughly denied subsequently by those who favor muscle dysfunction and/or psychosocial factors.
It is not certain who first applied the label “Costen’s Syndrome,” but it was not Dr. Costen.2 The label Costen’s Syndrome was first replaced by the label Temporomandibular Joint Syndrome (TMJ of unknown etiology).3 Then the psychological aspects of TMJ syndrome were studied,4–6 which eventually led to the proposed theory of the Myofascial Pain Dysfunction Syndrome (MPDS) by Laskin in 1969,7 presuming a psychological stress-related etiology. MPDS has never been definitively established by valid research as a primary factor. At the same time other authors were considering joint8 and muscular9 etiologies. This led to the suggestion that a differential diagnosis might be needed,10 which has continued to gain favor up to the present.11
In the early 1980s the label Temporomandibular Disorders12 (TMD = plural) was proposed by the ADA’s President’s council after presuming the presence of a multifactorial etiology. Forty or more distinct conditions have been identified.13 In 1992 the concept that TMDs are due primarily to psychosocial factors and illness behavior was re-proposed.14 However, to date there are no studies demonstrating the successful use of cognitive behavioral therapy or any other psychological method to exclusively treat TMD. Psychosocial factors do have support as perpetuating factors.15 Starting from about the same timeframe (1991), numerous studies have revealed an occlusal adjustment technique (Immediate Complete Anterior Guidance Development). This can be successfully applied to carefully selected sub-set, “occluso-muscle disorder” patients,16–23 a sub-category of TMD with primarily painful muscular symptoms.
There is currently a large separation between those who favor a psychosocial etiology and those who favor various physical etiologies. The etiologies currently vying for acceptance are; 1) psychosocial factors, 2) occlusal factors, 3) TMJ factors, 4) muscle factors, 5) skeletal factors, 6) centrally mediated pain and 7) combinations of these. Each TMD camp has applied different aspects of modern technology in their efforts to establish their preferred etiology. Since the symptoms of TMD are so diverse it is rational to expect that more than one etiology may be present in many cases. However, it is difficult to test these theories due to the diverse plethora of conditions that exist within the category TMD. The problem is, randomly assigning treatments to a heterogenous patient group predictably leads to equivocal results.24 This is compounded when a less than precise diagnosis is applied. It is especially important to determine an accurate diagnosis of the specific condition(s) for any TMD patient because there are many but not yet any “One Treatment for All.”25
2. Technologies that Aid TMD Diagnosis
There are only three sources of information from which a diagnosis can be made; 1) the history, 2) the clinical examination and 3) various physical measurements. Usually these sources tend to support one another, but not always. It has been previously shown that a history and clinical examination by themselves are too often not sufficiently precise to accurately indicate all of a TMD patient’s conditions.26–29
2.1 Technology that can be applied to the medical/dental history
The long-standing approach to collecting a patient’s history has been to provide a list questions for the patient to answer and perhaps a graphic on which to mark their areas of soreness, pain or discomfort.30,31 This method of collecting the patient’s history has continued to the present. Although the process is marginally efficacious, it has been made far more efficient with the application of computers and intuitive software. Computers have saved significant doctor time and reduced the amount of effort required from the patients too.32,33 The careful dentist treating TMD patients will also review the history with the patient. This is to make sure that the patient understood the questions and to verify a complete understanding of the patient’s responses.
In addition to the physical history some clinicians also include questions to evaluate the emotional history and current emotional status. It has been well established that TMD patients have higher levels of depression and somatization than asymptomatic subjects.33–36 Only recently supported by any research, is that the emotional factors may be only secondary to the common painful physical conditions.37 To date, no study has demonstrated a purely psychological method that can successfully treat TMD patients without some physical treatment component.38 Several computerized software tools are readily available to evaluate the depression levels of the TMD patients; the Beck Depression Inventory II, the Life Experience Survey, the Impact of Events Scale and the SCL-90 subscales.39–41
2.2 Technology applied to the clinical examination
The clinical examination of TMD patients varies considerably from the cursory to the highly comprehensive which includes subjective and objective data.42,43 The absolute minimum for an examination includes;
-
Millimeter ruler measurements and the observation of the range of motion (unassisted and assisted), whether pain is present in the TMJs and the amount of overbite
-
Palpation of TMJs to detect pain and/or “clicking or coarse/fine crepitus” and whether any present joint sounds are reproducible
-
Measure dental midline deviation or deflection if greater than one millimeter
-
Palpation of the masseter, the temporalis, the posterior digastric, all submandibular muscles, the lateral pterygoids and the temporalis tendons
The above considerations are usually just sufficient for screening new patients, but not for arriving at a definitive diagnosis when a patient is seriously symptomatic. Due to the phenomena of trigger points and referred muscle pain, clinicians that regularly provider TMD treatment are more comprehensive in their examination of patients.44 (e.g. The sternocleidomastoid muscle can refer pain to the temporalis in the form of a temporal headache.) The teeth, gingiva, mucosa, all of the head, neck and shoulder muscles and skeletal posture can be evaluated by an experienced clinician. Highly competent TMD treatment providers have found that additional time spent on diagnosis provides a more definitive initial treatment plan that produces faster patient responses and more effective final outcomes.
There are some computer programs available to assist with the clinical examination process and in some cases generate a report.45 Any clinician who plans to specialize in TMD treatment should take advantage of every tool that is available to minimize the numerous frustrations associated with caring for patients in chronic pain.
2.3 Imaging and other technologies applicable to the TMJ
Imaging is usually not routinely included in TMD screening evaluations but is more often requested when a patient’s TMJs are overtly symptomatic. Some suggest that imaging should only be included when “indicated.” This author has not found any standard “indications” or criteria in the entire dental literature for when imaging is truly warranted.
2.3.1 Panoramic X-rays
A high-quality panoramic x-ray is a good starting point when looking for the presence of any TMD or other pathology. While it is not a highly definitive indicator specifically of actual TMJ pathology, a normal appearing panoramic x-ray can aid the process of elimination of other potential conditions. See Figure 1. Panoramic x-rays are typically more readily available and less costly than the more sophisticated MRI or CT scans. A clear panoramic x-ray can also point to the need for a more definitive image or indicate that it is probably not needed.
2.3.2 Magnetic Resonance Imaging
MRI is considered by many as the one “gold standard” for imaging the TMJ. Of course, any image still requires proper interpretation. Few radiologists are trained to interpret TMJ images but most are very eager to learn what a dentist is interested in seeing. It is ideal to meet with your own radiologist and review dental interpretation of the TMJ together. See Figure 2.
Besides detecting the morphology of the joint and the disk position, a T2 weighted or STIR MRI can reveal the presence of inflammation and effusion in the TMJ. Some errors include; a) not having the patient open to max for the open view, b) poorly positioned slices that do not reveal the pathology, c) uncorrected views and d) assuming that the posterior band of the disk must be at an exact position when the mouth is closed. There is significant variation in form within the TMJ, making the determination of disk displacement sometimes a judgement call. There are also partial disk displacements (typically rotational) that are easily overlooked on an MRI.
Minimum Recommended MRI Views*
-
Proton Density, mouth closed, corrected sagittal projection, right and left TMJ. 8 or more views: lateral to medial, 4 cuts through condylar head.
-
T2 scan mouth closed, with corrected sagittal projection, right and left TMJ. 8 or more views: lateral to medial, 4 cuts through condylar head.
-
STIR (T1 inversion recovery) with corrected sagittal projection, right and left TMJ. 8 or more views: lateral to medial, 4 cuts through condylar head.
-
Proton Density, with mouth closed, corrected coronal projection, right and left TMJ. 8 or more views: in front of condylar head, through condylar head, behind condylar head. Be sure to show at least one slice anterior and at least one slice posterior to the condylar head.
-
Proton Density, mouth open fully, corrected sagittal projection, right and left TMJ. 8 or more views: lateral, medial, 4 cuts through condylar head. Make sure mouth is at maximum opening. Take this view last.
* Recommended by Drs. Ed Zebovitz & John Droter
MRIs are not very good at depicting early degenerative changes in bone. If the destruction of the condyle is sufficient, it will be evident on the MRI image, but subtle changes can be missed. In general, an MRI is most useful for detecting internal derangements and soft-tissue changes, while a CT scan is more appropriate for imaging changes in bone. These two technologies actually do complement each other, yet cost is a consideration. It is preferable to determine in advance if either image will be likely to reveal significant new information regarding the patient’s symptoms.
2.3.3 Computed Tomography scanning, Cone Beam Computed Tomography (CBCT)
The development of tomography created a more linear x-ray image with less ionizing radiation. The addition of a computer added the possibility of allowing the viewer to adjust the slices and consequently the views. The relatively recent development of the newer Cone Beam Computed Tomography machines has reduced the radiation exposure 96 % lower than for previous medical CT scanning. It has also lowered the cost of obtaining the images. Although the CBCT is not accurate for measuring bone density, the acquisition of 3-Dimensional anatomical datasets of voxels has been very useful in oral surgery, endodontics, orthodontics, implantology, and for 3-D imaging of the TMJ. See Figure 3.
More recently the pharyngeal airway space of patients with sleep disorders has frequently been imaged. See Figure 4.
With a long-term chronic but well adapted non-reducing displaced disk, the posterior attachment tissue can provide a cushion between the condyle and eminence that appears as if the disk is in place. Since the soft tissue and connective tissues are not visible, a false normal interpretation of the joint condition is possible. Before ordering a CBCT many TMD providers will look for any evidence of bone damage in the TMJ such as an opening deflection, a grating sound in the TMJ, an anterior open bite or a distinct facial asymmetry.
2.3.4 TM Joint Vibration Analysis (JVA)
One of the most common group of symptoms exhibited by TMD patients is TM Joint noises. Different conditions produce different noises with distinct frequency and duration profiles. This physical phenomenon has allowed the development of hardware and software that analyzes TMJ noises to scan for possible damage. JVA is not an alternative to TMJ imaging. It is complementary to imaging in that it can assist the TMD clinician in deciding whether MRI or CBCT will be more beneficial to the diagnostic process. In some cases where TMJ function has been determined by JVA to be within normal limits, neither image may be justified for a particular patient. JVA is 96% accurate when determining normal.46
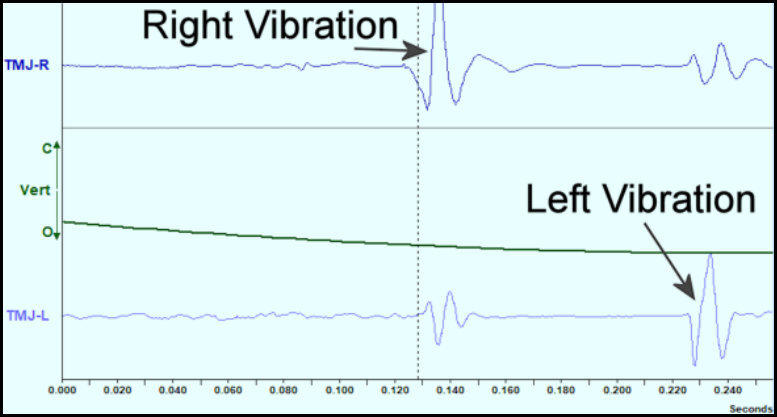
JVA sensors are placed over the TMJs bilaterally and held in place with an audio headphone style headband. See Figure 5. A ten-second recording is made while the patient is opening to maximum and closing to tooth contact 6 times following a metronome. The sensors are connected to a small amplifier which is connected through USB to a computer. The left and right vibration signals are digitized and displayed on the computer screen in a time sequence. Figure 6 shows vibrations in both the left and right channels. Figure 7 displays some typical waveforms of vibrations and indicates that the first vibration in each cycle is a right TMJ vibration and that the second vibration in each cycle is a left TMJ vibration. By averaging several vibrations together from different cycles, it is possible to quantify the intensities of the vibrations in each joint separately.
Figure 8 shows the intensity (Total Integral) of each vibration and the amount transferred to the contralateral side. The intensities and waveforms of both the right and left vibrations indicate bilateral reducing disk displacements.47 The percentage of transfer indicates the direction of the displacement of the disk.48 Approximately, transfers of less than 33 % are associated with anterior disk displacements. Those vibrations that transfer 33 % to 66 % are associated with antero-medal disk displacements, while vibrations that transfer more than 66 % are associated with medial disk displacements. All of the clicking, popping sounds and more subtle movements of the disk within the TMJ appear as short duration, relatively high amplitude vibrations that are easily recognized.
Degenerative changes within the TMJ cause surfaces to roughen and consequently produce very different waveforms and sounds, sometimes referred to as crepitus. When viewed on a computer screen the waveforms produced by degenerative joint disease are quite distinct. See Figure 9. The duration is much longer, often encompassing the entire opening or closing movement and the amplitude is usually much lower. The other striking difference is related to the frequency content. With degenerative vibrations the frequencies contained extend above the 300 Hz reference, but for disk movements a majority of the energy is below 300 Hz. See Figure 10.
The primary objectives of JVA are to detect any TMJ damage, distinguish between disk displacement or degenerative changes and to assess joint stability. This can be very helpful in determining whether imaging may be useful and if so, which imaging may be the most revealing. It is not always possible to arrive at a definitive diagnosis just with JVA but in some cases that is possible. The interpretation of JVA is very abstract even though the data are objective and quantitative. Initially, the learning curve is steep, but with experience, additional subtleties of interpretation are recognized. Thus, for screening new patients, for determining a need for imaging and for selecting between MRI and CBCT, JVA is effective.
2.4 Technology that is capable of evaluating movement disorders; electrognathography
Movement disorders can be systemic (e.g. ALS, Parkinson’s, etc.) or due to dysfunction in a limited area of the body. In dentistry the movement of the mandible is of primary concern, especially when the movement is limited or includes deviations. Three of the most common measurements are; 1) the range of motion (ROM) of the mandible when opening maximally, 2) the left and right lateral excursions and 3) protrusion. The normal ROM for males is about 55 mm (+ 5 mm) and for females about 5 mm less. The minimum ROM that is considered acceptable for masticatory function is about 40 mm. The clinician should consider the size of the individual since petite females may only open 40 mm with perfectly normal TMJs, which is still within 2 standard deviations and the 95% confidence interval for females.
Lateral excursions from centric occlusion should extend from 7 to 12 mm proportionately. When the translation of the condyle is restricted unilaterally, the lateral excursion to the contralateral is limited. Although limitation in lateral excursions can theoretically be due to muscular spasm, in most cases it is related to a non-reducing displaced disk blocking the anterior translation of the condyle. In a chronic condition, the effect of limitation is less than for an acute condition. When the condition of bilateral non-reducing displaced disks is present, the lateral excursions will be limited in both the left and right directions but may not be equal. The joint that is more chronic will usually translate farther.
Protrusion and protrusive guidance are not required for mastication, which occurs mainly as a frontal plane motion with very small sagittal component. However, speech movements occur mostly in the sagittal plane and very close to the protrusive guidance limits. The paragraph “My Grandfather” includes all of the phonetic sounds of the English language and can be used to generate an envelope of speech motion for any patient. This is handy for prosthodontists who are reconstructing a full mouth, but not particularly relevant to TMD diagnosis and treatment.
2.4.1 Measuring ROM with a millimeter ruler, a Boley gauge or a pair of calipers
The very simplest approach to measuring the ROM and the lateral excursions of a TMD patient is to use a ruler, a Boley gauge or a pair of calipers. There are some disposable devices made specifically for those measurements. See Figure 11. The amount of any anterior overbite is added (or open bite subtracted) and this is usually sufficient to determine the ROM value when screening new patients. This measurement can be established as part of a standard clinical examination. The lateral excursions are then measured with respect to the dental maxillary midline. While large deviations and deflections during opening and closing may be observed, they are not measurable with rulers, Boley gauges or a pair of calipers.
2.4.2 Electronic Pantographs
Mechanical Pantographs were originally developed to measure the condylar determinants of occlusion, which were transferred to an articulator for prosthetic reconstruction. Electronic pantographs have now replaced the mechanical ones for the same purposes. However, some authors have used them to record deviations in the condylar path during opening and closing in TMD patients.49–51 These deviations are distinctly different in patients with reducing disk displacements or non-reducing disk displacements. The clinical limitation of pantographs is the time it takes to apply them. While the ROM and lateral excursive activity can be measured very quickly with a ruler, the setup time for applying an electronic pantograph can be 30 – 40 minutes. Depending on the situation the additional information may or may not justify the additional time spent.
2.4.3 Video camera-based Jaw trackers
The currently available camera-based motion trackers (e.g. Sicat Function, CMS-JAW, Vicon MX, etc.) provide data with 6 degrees of motion; 1) vertical, 2) antero-posterior, 3) lateral, 4) Yaw, 5) Pitch and 6) Roll. This approach allows the system to track by extrapolation any point on the mandible including the condyles. These devices are used by those who are particularly interested in observing condylar motions. A search of PubMed for "video jaw tracking and TMD’ returned no published articles. A search of “video jaw tracking” returned seven articles, none related to TMD. The limitations of using this type of jaw motion tracker for TMD motion analysis are; 1) a mandibular clutch must be attached to the mandible, 2) the setup time is significant, 3) these systems are very expensive and 4) limited software is available that is ready to use for jaw tracking.
2.4.4 Permanent magnet-based jaw trackers
Permanent magnet-based jaw trackers have been commercially available since the mid-70s. They track a small permanent magnet placed in the labial vestibule that is attached to the mandibular incisors; 1) vertical, 2) antero-posterior and 3) lateral. The most important features of magnetic jaw trackers are; 1) no clutch on the mandible, 2) quick setup and 3) patients can masticate naturally without any interference. Software has been continuously developed since the mid-80s and is currently very sophisticated. In addition to measuring the ROM and lateral excursions, there are eight additional measurements available:
-
Lateral and antero-posterior incisal deviations and/or deflections during ROM opening
-
The incisal location of a disk reduction during opening when used with JVA
-
Incisal freeway space from rest to occlusion
-
The incisal velocity of all motions
-
Incisal movement and the maxillo-mandibular relationship during swallowing
-
The opening, closing and occlusal times during mastication
-
The shape of the Average Chewing Pattern (ACP) during mastication
-
The smoothness or jerkiness of chewing motions
The magnet is applied to the patient with Stomahesive, the tracker array is placed upon the head and aligned to the magnet within just a few minutes. See Figure 12. The quick setup and minimal per use cost are characteristics that promote widespread clinical use. When the jaw tracker is ready to record, the first trace taken is a ROM. When the recorded ROM trace agrees with the previously taken manual measurements the alignment is verified. For example, if a TMD patient suffers from a unilateral non-reducing disk displacement (closed lock) a deflection towards the affected side will both be observed and recorded at maximum opening. See figure 13.
If instead the TMD patient’s displaced disk reduces during opening, an opening deviation towards the affected side will return to the midline or perhaps a little beyond at maximum opening. See figure 14. After the ROM trace is verified, left and right lateral and protrusive measurements can be recorded as well.
The location of the deviation due to reduction can be significant with respect to treatment of a reducing displaced disk. An early reduction is more likely to be recapturable than a mid to late reduction. When using a jaw tracker together with JVA the combined technologies provide stronger evidence of the patient’s current TMJ condition. This can be helpful when devising a treatment plan, specifically with respect to TMJ internal derangements.
To measure the freeway space, it is first necessary to encourage the patient to relax and allow the mandible to rest. Although it is usually easy with a normal subject, it is not always so with a TMD patient. Some TMD patients clench and grind their teeth together even during awake times. Others posture their mandibles near centric occlusion in anticipation of the need to swallow approximately 3,000 times/day. If a skeletal maxillo-mandibular mal-relationship exists, the patient will use their musculature to compensate and posture the teeth near the maximum intercuspal position (MIP). To relax the musculature, it is sometimes necessary to first reduce the inherent proprioception. This can be done with ultra-low frequency transcutaneous electrical neural stimulation (ULF-TENS at 0.5 to 2.0 Hertz). Once the patient is at a relaxed rest position a simple closure into the MIP will suffice to accurately measure the real freeway space. The patient at rest is instructed to close, tap and protrude. See Figure 15.
The velocity or speed and smoothness of motion can be an indication of confidence or the lack thereof in the movement. It is particularly evident during closure. A tentative closure slows down as it is approaching the occlusion, which can be demonstrated by instructing the patient to “open wide and close fast.” See Figure 16. When a patient is unable to produce a fast closure, it usually indicates muscular compensation and/or uncertainty on the part of the patient. Pain in the joints and/or muscles can also be a factor in slowing down the motion. However, pain in the musculature often results from some awkward muscular compensations. The masticatory system functions as a whole complex entity. Dysfunction in any part of it will reduce the quality of the whole system’s function.
Swallowing occurs frequently enough that the central nervous system (CNS) maintains an anticipatory status of the musculature, ready to swallow anytime. The most normal swallow occurs with the teeth in contact (or against a hard bolus) for stability, but swallowing can occur with a portion of the tongue between the teeth. The tongue can be used to compensate for a maxillo-mandibular mal-relationship and make swallowing easier and more comfortable. A record of a patient’s type of swallow can be made by starting at rest, instructing the patient to swallow and then close into MIP. See figure 17.
A tongue thrust swallow is not necessarily problematic, but should be noted if orthodontics or other procedures that may alter the occlusion are anticipated. When a patient is TMD symptomatic and has a tongue swallow, the maxillo-mandibular relationship should be carefully evaluated.
One of the important requirements for good health and quality of life is the ability to masticate effectively. It is important both for patient comfort and good nutrition. Poor mastication can often lead to gastrointestinal conditions such as the common irritable bowel syndrome (IBS), gastroesophageal reflux disease (GERD), diarrhea, constipation, and poor nutrition. Loss of teeth is the most obvious factor affecting mastication, but TMD can also reduce the quality of a patient’s masticatory function.
The rate of chewing or cycle time is one indication of the quality of masticatory function. The mean normal cycle time is nominally about ¾ of a second. As mastication becomes more and more dysfunctional, the cycle time increases, extending to longer than one second/cycle. However, if a dysfunctional condition such as a TMJ internal derangement becomes very well adapted, the cycle time typically returns to within the normal range (0.5 to 0.9 seconds). Subsets of the cycle time include; 1) opening time, 2) closing time and 3) occlusal time. Measuring all of these times can aid in the understanding a TMD patient’s specific condition. See Figure 18.
When the cycle time is extended it is due to the extension of one or more of these subset times. If the patient has difficulty opening due to a reducing displaced disk, the opening time will be extended. Likewise, if there is difficulty approaching the MIP the closing time will be extended. Another measurable change that occurs as a result of dysfunction is an increase in the variability of the timing. The timing standard deviations (SD) from a normal control subject are typically less than or equal to 0.05 seconds (50 milliseconds) for the opening, the closing and the occlusion times while the total cycle time SD can be somewhat longer.
Another factor that varies with the quality of masticatory function is the shape of the average chewing pattern (ACP). This pattern is created by averaging 10 to 20 chewing cycles in three dimensions at the incisor point. Mean normal patterns have been calculated from a control group of 500 normal subjects.52 When TMD patients have difficulty chewing their ACP diverges from the normal pattern. See Figure 19.
However, if a dysfunctional patient adapts well to an internal derangement their ACP may improve back to a nearly normal pattern. A worn dentition will exhibit a flattened and broader ACP, but any restriction in the occlusion will narrow the ACP. A close to normal pattern suggests good function, but does not preclude muscle pain since the TMD patient may still be struggling muscularly to produce a nearly normal ACP. Consequently, it is necessary to also evaluate the muscle function before concluding that the system is functioning in a completely normal manner. Muscle function will be reviewed in section 2.5.
Another measurable factor related to the quality of masticatory function is the smoothness of the chewing pattern. Good function is smooth, but jerkiness increases in proportion to the degree of dysfunction. “Jerk” is the third derivative of movement and can be evaluated using calculus (d3s/dt3) with units in meters/s3. It is not quite as simple as that, however, because well adapted TMD patients tend to be jerkier than poorly adapted TMD patients. The reason is that poorly adapted TMD patients chew very cautiously, while better adapted TMD patients tend to chew at a normal rate. Long cycle times are associated with poor adaptation, increased jerkiness with better adapted conditions, all else being equal.
2.5 Technology that is capable of evaluating muscle disorders; electromyography (EMG)
Electromyography records the electrical activity from a muscle as it contracts. The voltage present is very small (measured in microvolts, millionths of a volt), which requires a special differential amplifier to record it. There are two approaches to recording EMG data.
2.5.1 Using a bipolar needle
A bipolar needle (invasively) inserted into the muscle of interest, as the electrode, it is possible to be very specific to just one muscle. Needle electrodes record from a very limited area of a muscle and tend to produce some artifacts with movement. Needles are excellent when used for recording single fiber motor unit potentials (MUPs) at low levels of contraction, which are useful for detecting the presence of a myopathy or a neuropathy. Systemic neurologic and muscle diseases are diagnosed and treated by medical doctors, not dentists. Thus, needle EMG is the favored approach of neurologists. In contrast, dentistry is more interested in muscle function.
2.5.2 Surface EMG
The main alternative to needle EMG is the use of surface electrodes. Surface EMG (sEMG) is non-invasive and much easier to implement. Bipolar electrodes are simply adhered to the skin over the muscles of interest. The bilateral muscles of greatest interest to dentists are; 1) the superficial masseter, 2) the anterior temporalis, 3) the suprahyoid area (under the chin) and 4) the sternocleidomastoid for head posturing. See Figure 20. The axes of the bipolar electrodes are approximately aligned with the fiber direction of each muscle. The signals recorded represent a much larger area of each muscle than with needles, but some signal leakage from adjacent muscles is also common. For the masseter and temporalis muscles the adjacent muscles create facial expressions, making it important that the patient maintain a passive facial expression. For the suprahyoid area, there are several muscles close together, but the main objective in that area is to observe a lack of activity in all of them. Any adjacent activity does not represent a significant interference when strong contractions are present, but can be for light contractions. There are five specific types of records are typically recorded:
-
Resting or posturing activity
-
Swallowing activity
-
Maximum voluntary clench
-
Clench on cotton rolls (or another object between the teeth)
-
Chewing a soft or tough bolus
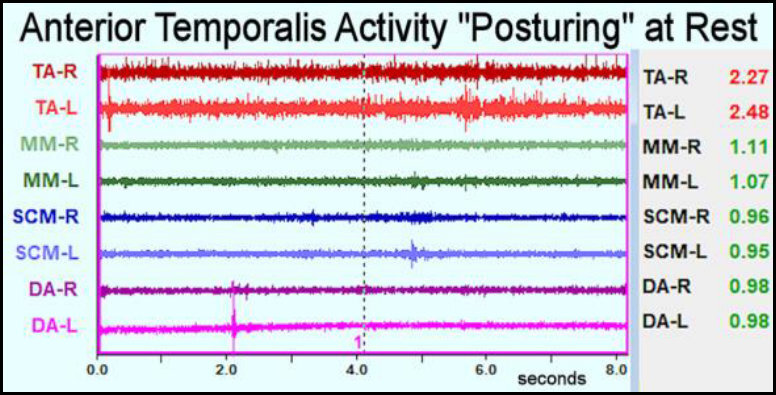
It has been understood for many decades that when a muscle is at rest the normal activity level is extremely low or quiet.53 Thus, under normal circumstances the elevator muscles do not need to maintain the posture of the mandible at rest. However, some TMD patients have elevator muscles that are actively posturing the mandible at “rest.” See Figure 21. The reason we know that it is masticatory muscle activity rather than facial muscle activity is because when the activity is removed by applying ULF-TENS, the vertical dimension of rest increases.54 No facial muscle can alter the vertical dimension of rest. The best explanation for why the posturing activity is present in some TMD patients is a maxillo-mandibular mal-relationship. The muscles are simply compensating for the mal-relationship by posturing the mandible near MIP. Even low levels of activity if maintained continuously can lead to muscle pain.55,56 The explanation for the pain development mechanism appears to be a gradual reduction in metabolites within the muscle and the accumulation of lactic acid during static low-level contractions.
Swallowing activity can easily identify the two most common swallow types; 1) swallowing in MIP with the teeth in contact or 2) placing the tongue between the teeth during a swallow. See Figure 22. Although a tongue-thrust swallow is not necessarily pathologic, it is usually a rather good indication of a maxillo-mandibular mal-relationship, almost by definition. Since the tongue-thrust swallow is an adaptive mechanism it should not be surprising that many such subjects do not have painful muscles. However, if orthodontics or major reconstruction are being considered, it is helpful to record the patient’s swallow.
The maximum voluntary clench (MVC) is a test of both the strength of the elevator muscles and an indication of the balance between them. There are several reasons why a clench can be weak or unbalanced; 1) a sore tooth, 2) one or more missing teeth, 3) muscle fatigue, 4) some poorly arranged occlusal contacts or 5) a skeletal mal-relationship of the mandible to the maxilla. Any one or a combination of these factors can alter the ability of individual muscle to function. EMG can demonstrate the current muscle function situation very succinctly. See Figure 23. To differentiate between weak muscles or the other conditions it is customary to place cotton rolls or similar over the posterior teeth and repeat the clench. If there is no change, the muscles are probably weak. If with the cushioning the activity increases to near normal levels, one or more of the other conditions are likely.
Ultimately, good masticatory function should be a primary goal, especially for those TMD patients with functional limitations. Good muscle function can be determined as easily as good TMJ function and good occlusion. While it is possible to have poor muscle function and good TMJ function, the reverse is never true. When there is any deterioration TMJ function, the CNS will use the musculature to compensate. Thus, every patient with TM joint dysfunction will also have muscle dysfunction. If both joints are in good order, then either the occlusion or the maxillo-mandibular relationship can cause muscle dysfunction. Muscle pain is very common in TMD, but myopathy and neuropathy are not anywhere near as common. Thus, TMD muscle pain is most often due to compensatory activity. Treating the muscles requires treating the TMJs, the occlusion or a skeletal mal-relationship. Alleviate the joint, occlusal and skeletal problems and the muscles will usually respond favorably.
Mastication is normally a unilateral activity with unbalanced activity of the elevator muscles. The normal hierarchy of activity is; a) the working masseter is most active, b) the working temporalis is next, c) then the non-working temporalis and 4) finally the non-working masseter. See Figure 24. The quality of masticatory function can be evaluated by recording the jaw motion and EMG muscle activity simultaneously. With respect to jaw motions, good performers generally chew faster, with larger vertical and lateral components and with less variability.57,58 With respect to good masticatory muscle function, good performers produce high strength short bursts following the normal hierarchy that peak before the end of closure.22 In contrast, dysfunctional subjects chew more slowly with their muscle activity often peaking after the end of closure, with lower amplitude bursts that last longer and with higher variability. One of the common compensatory differences between normal control subjects and dysfunctional patients is high activity of the non-working masseter muscle. See Figure 25. This type of pattern means both masseter muscles are working all of the time, whereas with normal function, the non-working side masseter rests.
2.6 Occlusion analyzing technologies
The role of occlusion in TMD has been controversial for many decades. There has been no significant correlation between the Angle’s classification of occlusion and the development of TMD. This means that Class I occlusions are equally at risk for developing TMD as are all other classifications. Most of the other occlusal variables, CR – CO slides, overbite, overjet, etc., have also been discounted as contributing to TMD.59 However, the deliberate introduction of occlusal interferences to function (e.g. simulated high fillings) has been shown to disrupt the masticatory system and initiate some TMD symptoms.60,61
2.6.1 Occlusal marking paper, silk, etc.
For many decades the standard approach for occlusal adjustment has been to mark the teeth with ink from paper or silk and then adjust the occlusion according to one of the popular philosophies. The marks on the teeth correspond to contact locations, but do not indicate either the timing or the force of the contacts. It was once thought that larger paper marks or ones with a particular shape might indicate higher force. However, this notion has been formally denied.62–64 The only possible determinations with paper/silk marking are to establish each tooth contact’s approximate size and location, not the force or timing of any contact. While conventional occlusal adjustments were once a very popular Gnathological treatment for TMJ dysfunction syndrome, but they gradually fell out of favor in the 1980s.
2.6.2 Occlusal indicator wax (Kerr Corporation, Orange, CA)
The application of occlusal indicator wax was conceived originally by Dr. Bernard Jankelson to allow a more 3-dimensional indication of the occlusal contacts. The green wax has a degree of translucency that reveals when an “almost contact” exists. When adhered to the teeth it also allows the patient to “eat the wax” with a few closures in an attempt to identify any interferences to closure that might occur on vertically sloping cuspal inclines during mastication. While it adds somewhat to paper marking, it still lacks force and timing.
2.6.3 T-Scan Digital Occlusal Analysis System (Tekscan, Inc., South Boston, MA)
In the mid-1980s the first generation of the T-Scan system was developed and offered for sale commercially.65 The initial model was very limited in capability and did not perform very well. Subsequent models increased the resolution of the digitizing, upgraded the sensor wafer several times for greater reliability and converted the system to be operated through an IBM compatible personal computer system. By utilizing the personal computer, the software development capabilities were greatly enhanced. The current generation has the benefit of more than three decades of software and hardware research and development.
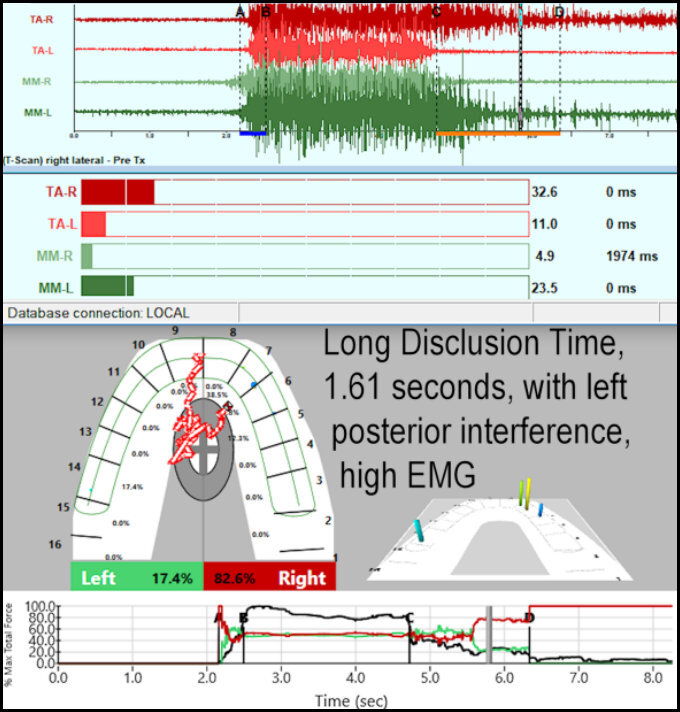
While the T-Scan does not mark the teeth, it does allow the dentist to see the distribution of relative forces around the arch and the timing of the contacts. The timing function is used to evaluate the closure into MIP and for the timing of lateral excursions.16,19,21,23 The relative distribution of forces is used to balance the natural bite into MIP17,18 and to delay the loading of an implant supported prosthesis.66 See Figure 26.
When using the T-Scan to adjust an occlusion to remove interferences to masticatory function a procedure, immediate complete anterior guidance development (ICAGD), has been extensively tested.16,21,22 This procedure reduces the lateral excursive disclusion times to less than 0.5 seconds, by eliminating both ipsilateral and contralateral posterior contacts during lateral excursions. See Figure 27.
This approach combines T-Scan and EMG measurements and minimizes the amount of muscle activity required during masticatory function.23 It is also effective in reducing tooth sensitivity to cold water swish.67 The amount of tooth structure removed is minimized by targeting only those teeth that are indicated by the precise measurements. Although the T-Scan has been criticized in a few invalid bench tests published in the literature (e.g. cutting the sensors in half, using raw sensel data, etc.), none of the published critiques to date has applied the T-Scan in vivo to actual patients.
SUMMARY
The multiple etiologies of TMD are almost always physical and most often involve joint problems, occlusal problems, skeletal mal-relationships or some combination of these. The symptom set is highly variable and dependent on each unique individual’s situation. The real emotional factors are most often secondary to painful physical conditions, not the cause of them. No purely psychological treatment has yet been devised to successfully treat TMD without concurrent physical treatment.
The ultimate in futility results from the mistaken assumption that one diagnosis or one treatment (e.g. Michigan Splint, NTI, Botox, Opioids, etc.) can be applied to all TMD cases. Nothing is more valuable for the treatment of TMD than obtaining a precise comprehensive diagnosis, which can lead to a successful treatment plan. The “trial and error” approach, too often advocated, is prone to random failures or limited successes. In contrast, a precise diagnosis allows the clinician to develop a logical plan that will most often sufficiently improve or completely eradicate the patient’s specific complaints. The astute TMD provider uses the technological advantages available in a cost-effective and appropriate manner to maximize the improvement in each patient’s welfare. TMD technologies provide the greatest advantage to the new inexperienced provider who does not have many years of practice treating TMD.
Acknowledgments
Dr. Robert Kerstein, Dr. Gerardo Ruiz-Velasco, Dr. Manminder Sethi, Prof. Prafulla Thumati and Dr. Robert Kull provided all of the clinical data presented in this chapter.
Potential Conflict of Interest
John Radke, BM, MBA is the Chairman of the Board of Directors for BioResearch Associates, Inc.
Thanks
To all of these past mentors. Very little of what has been presented here originated solely from me. These ideas have been discovered and refined incrementally by these innovative past and present contributors to clinical dentistry; Yojiro Kawamura, Charles Stuart, John R. Thompson, Bernard Jankelson, Hiroshi Mitani, William Farrar, Harold Gelb, Atsushi Yamashita, Arthur Lewin, Takao Maruyama, Lars Christensen, Jorge Learreta, and so many others.













_and_dysfunctional_(right)_velocity_patterns_opening_and_closing_fully.jpg)
_and_tongue-thrust_swallow_(bottom).jpg)
_and_normal_mastication_(bottom)__which_is_faste.jpg)
_of_dysfunctional_patient_(left)_and_normal_control_subject_.jpg)


_and_tongue-thrust_swallow_(bottom)_shows_an_inverted_.jpg)
__weak_unbalanced_emg_clench_(bottom).jpg)

















_and_dysfunctional_(right)_velocity_patterns_opening_and_closing_fully.jpg)
_and_tongue-thrust_swallow_(bottom).jpg)
_and_normal_mastication_(bottom)__which_is_faste.jpg)
_of_dysfunctional_patient_(left)_and_normal_control_subject_.jpg)

_and_tongue-thrust_swallow_(bottom)_shows_an_inverted_.jpg)
__weak_unbalanced_emg_clench_(bottom).jpg)