What is TMJ Joint Vibration Analysis?
Joint Vibration Analysis of the temporomandibular joint is the process of; 1) recording vibrations from within the TMJs through accelerometers, 2) evaluating the intensity and frequency content of the vibrations and then 3) comparing the values to known values from previously verified examples. Accelerometers are used because, unlike microphones, they can be precisely calibrated to express vibration intensity in Pascals. The vibrations are recorded while the subject opens and closes from the maximum intercuspation position (MIP) to maximum comfortable opening, exercising the full limits of the ranges of motion of both joints. For maximum value the mandibular motion can be recorded simultaneously to provide a precise indication of the degree of opening at the onset of any vibration, as well as the amounts of all deviations and or deflections present.
The recording is initially displayed as a “sweep” graphic showing the left and right vibrations along with the mandibular motion for several open and close cycles. See Figure 1.
In Figure 1 there appears a large vibration recorded from the left TMJ and a small vibration recorded from the right TMJ. The cursor (left edge of the display) can be positioned over the vibration to better view it and multiple iterations can be superimposed to reveal the consistency of the vibration. See Figure 2. Not only is the waveform consistent, the three-dimensional position of the mandible at the onset of vibration is also very consistent. Note: The small vibration recorded from the right TMJ is consistently occurring simultaneously with the vibration from the left TMJ, which suggests it is the same vibration transmitted through the mandible, not originating in the right TMJ.
To quantitatively evaluate the frequency content of the vibration a Fast Fourier Transform is calculated and displayed as a frequency distribution graph. See Figure 3. The similarity of the left and right frequency distributions further indicates that the small vibration recorded from the right TMJ is the same vibration originating within the left TMJ.
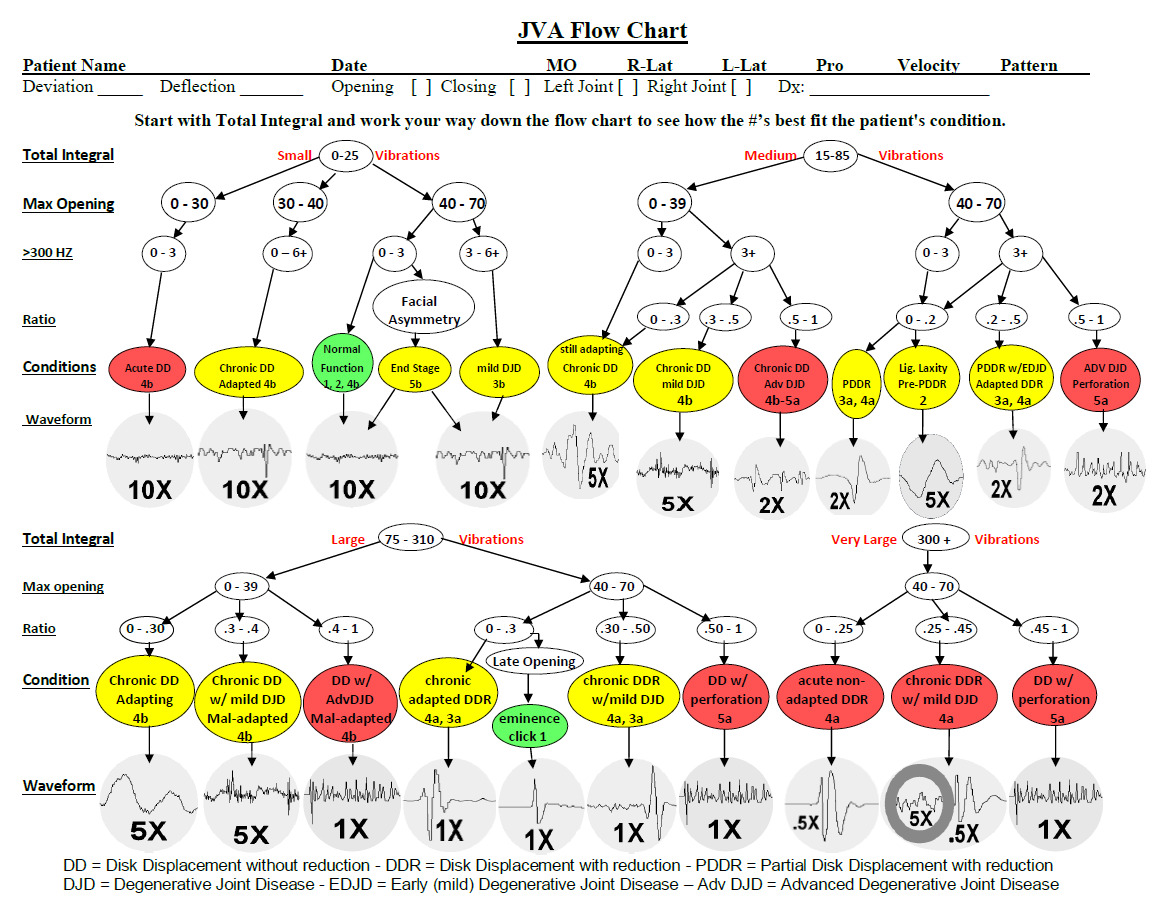
To simplify the interpretation of the measurements a JVA Summary of numerical values is displayed. See Figure 4. The values from the JVA Summary can be input to the JVA Flow Chart to find the most likely match. The most important parameters in order of merit are: 1) Total Integral (intensity), 2) maximum Range of motion, 3) the amount of the intensity that is represented by frequencies above 300 Hz (> 300 Hz Integral) and 4) the Ratio of the high frequencies to low frequencies (> 300 Hz / < 300 Hz). Other parameters can provide indications of the degree and quality of adaptation. To use the JVA Flow Chart it is only necessary to input these four parameters. See Figure 5.
The total time required to apply JVA is usually only a few minutes, there are no consumable costs included and the recording of the data is usually accomplished by auxiliary personnel (e.g. hygienist or assistant). JVA implementation even in a busy practice is minimal, but it demonstrates a higher standard of care to the patients, increasing the bottom line. There are no constraints with respect to ionizing radiation (CBCT), referral (MRI) or additional patient costs for obtaining repeat follow-ups post treatment. JVA does not compete with imaging because it provides very different information. While the MRI and CBCT images reveal important characteristics regarding the morphology of the TMJ, JVA records the quality of the function of both TMJs while they are in motion.
JVA usage in general does a superb job at accurately identifying patients with healthier joints, while conveniently categorizing those with less healthy joint status to be identified.
This introduces a systematic way for those who might require imaging to be conveniently identified in a busy and technically robust practice. Additionally, JVA allows for a permanent digital record of the TMJ joint status to be created within the patients chart, far superior to the subjective and crude recordings of popping, clicking, and simple range of motion notations that, even if recorded, are often of little practical use as the JVA research suggests.
What do three decades of dental literature say about Joint Vibration Analysis?
The specificity, the ability of Joint Vibration Analysis (JVA) of the temporomandibular joint (TMJ) to detect the presence of normalcy of TMJ function, has been shown to be about 98%.1 This indicates that JVA is by far the best screening tool available for detecting absence of TMJ disturbances in a clinical setting minimizing false positive indications. This capability is due in large part to the dynamic nature of JVA. Unlike static imaging, JVA is recorded with the TMJs exercising to the limits of their range. This allows measurement of both the range of function and the location of any obstruction to function. The importance of these dynamic measurements is related to fact that some internal derangements adapt successfully and result in good function (with no treatment indicated), while in other cases the TMJ degenerates and its function is severely compromised.
In a study using JVA to identify the presence of internal derangement of the disk with and without reduction, the sensitivities (detectability) were measured between 91.8% and 96.6%.2 In the same study disk displacement without reduction was somewhat less precisely detected, in about 77 % of the cases, due to the omission of Range of Motion as an important contributor to that diagnosis. However, it is more valuable for treatment planning to determine whether the temporomandibular joint is functioning relatively normally regardless of whether the disk has been displaced (MRI). Good function can re-occur after the posterior attachment tissue de-vascularizes, denervates and forms a scar tissue pad between the condyle and the eminence, protecting against the development of osteoarthritis. Some refer to this condition as a pseudo-disk, but no disk-like structure is formed.
The vibrations recorded from TMJs in different conditions have been shown to contain statistically significant differences in both their amplitude and their frequency distributions.3 When patients with degenerative joint disease were tested with JVA the successful detection rates (Sensitivities) were; a) 100% of the TMJs with disk displacement without reduction associated with DJD; b) 87.0% of the TMJs with disk displacement without reduction associated with perforation; c) 88.9% of the TMJs with disk displacement without reduction associated with DJD and perforation; and d) 100% of the TMJs with only perforation.4 JVA data has also been tested for reliability between sessions and between days and has been shown to be reliable.5,6
Some clinicians and academics claim that palpation is sufficient to detect internal derangements with sufficient reliability.7 However, the same authors have claimed that clinical signs are not stable indicators of TMD.8 There is a well-documented consensus that internal derangements are difficult to diagnose with clinical examination alone.9–22 It has also been found that basing a diagnosis of internal derangement upon the presence or absence of sounds through sonography is unreliable.14 Consequently, JVA uniquely provides an alternative screening capability that augments clinical examination at a tiny fraction of the per patient cost of sophisticated imaging such as MRI or CBCT.
JVA includes the convenience of an in-office procedure, provides an objective permanent record and it can be repeated as often as desired with zero invasiveness to follow the progress of treatment. Some dentists recommend annual records to monitor TMJ health just as one does periodontal health. It is an axiom of medicine that early detection is important for successful treatment. JVA has also been shown to complement CBCT and MRI imaging by predicting which type of image will more likely provide useful information for diagnosis after the presence of TMJ damage has been documented.23 In addition, JVA may help individualize the imaging diagnosis since similar lesions in different patients, may behave differently under function. In a similar manner, in the same patient, JVA recordings along the treatment may identify small changes of the TMJ status, that do not present enough structural changes to generate a clear imaging, such as early articular surface deterioration of the disc and condyle cartilage that impact friction, but do not yet have either sufficient signal intensity to induce proper imaging in the MRI coils, nor enough cortical bone density variation to generate proper CBCT imaging. Therefore, helping the clinician early on to address possible flare ups of a pathological condition or even monitor improvements of the joint function.
Of course, with the advent of every new technology there are always nay-sayers with opinions contrary to the published facts.24 It should be noted that those who have chosen to actually study JVA first hand, have subsequently changed their previous negative opinion and concluded that JVA is in fact very useful as an aid in diagnosis of internal derangements.6 It has also become apparent over the last three decades that a broad consensus has been reached with respect to JVA as it has become increasingly utilized as a screening test for TMD patients.25–58
Note: Electrovibratography (EVG) was the first term used to refer to the recording of vibrations originating within the TMJ. EVG was later changed to Joint Vibration Analysis, which is specific to the use of accelerometers to record vibrations, including inaudible vibrations.
Potential Conflicts
J Radke is the Chairman of the Board of BioResearch Associates, Inc. Dr. Ben Sutter reports no potential conflicts of interest.


_shows_the_frequency_distribution_as_well_as_the_consisten.jpeg)



_shows_the_frequency_distribution_as_well_as_the_consisten.jpeg)