Introduction
“Facts are stubborn things; and whatever may be our wishes, our inclinations or the dictates of our passions, they cannot alter the state of facts and evidence.”
John Adams 1770
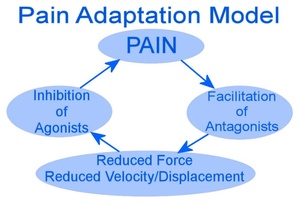
Two major competing paradigms have become mainstream that attempt to explain the changes in muscle that accompany pain. These are formally known as the Vicious Cycle Theory (VCT) and Pain Adaptation Model (PAM). In short, the VCT holds that muscle pain can develop from continuous muscle hyperactivity leading to fatigue. When the muscles relax the pain abates. In contrast, the PAM advocates that pain is the initiator and agonist muscles become hypoactive to minimize further pain or injury of the muscle. Antagonist muscles increase their activity. Also the resting level of the muscles is claimed to be no different in comparing normal to painful muscle activity.
The names of these opposing physiologic paradigms are revealing, as there are differences between a model and a theory. While these are subtle differences, the two terms are often used interchangeably even though they are not interchangeable. “Patterns of data may suggest theories and/or models, with the latter necessitating validation against facts. This form of scientific explanation therefore, moves from data to theory, from theory to model, and from model back again to data.”1 As such, data plays a pivotal role to strengthen or falsify both theories and models. This critical analysis will examine the primary literature from each paradigm, as well as assess both paradigms’ respective supporting literature. Since the behavior of muscle as the cause of pain is a central theme to both paradigms in the context of TMD, it is this authors contention that muscle activity must be recorded and compared, to offer any understanding of the actual occurring physiology.
Literature Review
The discussion on muscle function as it relates to pain within the dental literature has proven to be more academic than clinical or scientific. Scientific discussions involve the measurement with biometrics before and after rendering a treatment. The VCT was first promoted and named by Travell2,3 from her observations and later supported by Ramjford,4,5 who described that muscle hyperactivity resulted in dysfunction and pain. Figure 1. Ramjford’s study involved 34 patients who underwent EMG measurements pre- and post-occlusal adjustments.4 Specifically, non-working interferences were removed, and the working side group function was altered by recontouring existing working side interferences, creating excursive movement smoothness, instead of controlling the number of excursive tooth contacts. With these specific occlusal adjustments, the pre-adjustment observed muscle hyperactivity went down and symptoms resolved. Since Ramjford’s original work, improvements in a number of occlusal technologies have evolved that allow for bite force balancing and for bite timing reductions to be accomplished to very high levels of precision. Biometric technology also allows for real-time synchronization of occlusal contact forces with muscle activity levels. T-Scan 10 (Tekscan Inc. S. Boston, MA USA) synchronized with the BioEMG III (Bioresearch Associates, Inc., Milwaukee, WI, USA), can replicate what Ramjford was trying to accomplish, but much faster and with greater accuracy. Many T-Scan/BioEMG publications have shown that hyperactive muscles calm down once working and non-working interferences are removed to specific excursive movement time-durations and bite force equalization is established.6–23
Kerstein, Sutter, Thumati, Brattesani, Radke and Yiannios6–23 are just a few of the authors who have all reported similar findings. These specific citations were selected, as each author recorded pre and post therapy EMG levels of the bilateral temporalis and masseter muscles, and statistically analyzed the detected muscle activity level changes. The treatment being rendered was Disclusion Time Reduction (DTR), which has been described in detail in multiple publications since 1991.6 Briefly, all molar and premolar working and non-working excursive interferences are removed to reduce the excursive Disclusion Times to less than 0.5 seconds per excursion. These adjustments make the excursive movements both faster and smoother under complete anterior guidance control, while simultaneously balancing the overall bite force profile. DTR must be accomplished under specific protocols that can only be accomplished by utilizing a digital occlusion analyzer (T-Scan 10/BioEMG III) that can accurately record relative bite force, timing and muscle activity.
Post DTR, muscle activity decreased among these treatment populations with aggregate p-values ranging from 0.05 to 0.00001.6–23 These multiple repetitive treatment outcomes constitute more than just a theory. At this point, consistent unidirectional data from multiple providers performing DTR in different clinics on different patient populations moves the computer-guided occlusal adjusting from theory to an etiological relationship that strengthens the VCT. These many studies’ findings are important, as therapeutic improvements did not require the mandible be repositioned into Centric Relation (CR), nor did the participants require Transcutaneous Electrical Neural Stimulation (TENS) therapy to accomplish the reported muscle hyperactivity reductions.6–23
Four decades after VCT was hypothesized, Lund et al published the Pain Adaptation Model (PAM).24 Figure 2. This manuscript was an overall evaluation of skeletal muscle behavior during painful conditions. The authors included 119 citations involving cats, rabbits, elbows and other limbs, lower back pain, tension headaches, fibromyalgia, and post exercise muscle soreness, but only 8 Temporomandibular Disorders (TMD) articles that measured muscle function with EMG’s.25–32 A critical examination of this data is essential to understanding the underlying physiology that PAM hypothesizes; the pain comes first, which leads to muscle hypoactivity and that there exists no difference in muscle resting activity comparing normal and painful muscles.
Dahlstrom et al.25 clearly stated that treatment revolves around “the assumed etiology,” while there is a “theoretical assumption that general anxiety or tension is associated with increased muscle tension.” Given that assumption, 20 controls and 20 patients with mandibular dysfunction and unilateral pain in one masseter muscle had EMG electrodes attached over their masseter muscles while being asked to squeeze dynamometers in both hands for 1 minute. Next, subjects were asked to thread a thick thread through a small needle for 2 minutes. And lastly, each participant while blind folded, was asked to complete a puzzle in 2 minutes, where 1 piece was intentionally omitted. Table 1 re-drawn from Dahlstrom clearly shows the patients had elevated EMG activity pretreatment compared to controls and post therapy the patients had lower EMG activity than the controls. Although quoted by Lund as supportive, these results are in direct contradiction to the PAM theory because the muscles started out more hyperactive, became more relaxed post treatment and the authors reported higher resting muscle activity in painful patient muscles than in controls.
Majewski and Gale26 examined the EMG activity of anterior temporal area in pain and non-pain participants, initially examining patients with unilateral muscle pain. In their Materials and Methods, they state “Pain symptoms were not present at the time of the EMG measurements. We selected pain-free periods for better evaluation of the relation between increased muscle tonus and pain.” This is clearly a logical error because one would have to make EMG recordings in both pain periods as well as pain free periods, to evaluate the relation between increased muscle tonus and pain. The authors reported “no differences were found in the level of significance of the pain vs non-pain comparison in EMG raw values, or in the EMG percentage values.” No doubt the PAM authors zeroed in on this statement without understanding the study design, such that any conclusions the authors arrived at were meaningless due to the study’s design flaws.
Sherman27 evaluated masseter muscle surface EMG recordings in four patient groups; 1) pain free patients with no history or physical evidence of TMJ, 2) patients with clear TMJ problems but no history or evidence of bruxing or clenching, 3) patients with bruxing or clenching behavior, but no evidence of TMJ problems, and 4) patients who clenched and bruxed, with TMJ problems. The recordings were done in three sessions, each recording being 30 seconds long. In the first session, no patient instructions were given. In the second session, patients were asked to clench at the beginning of the recording but were allowed to relax towards the end. In the last session, the participants were asked to relax and “let the tension drain” with their mandible hanging down 1/8 of an inch out of MIP.
Displaying the raw data in a bar graph, the EMG levels trended up as group complexity increased. See Figure 3. Sherman’s classifications failed to quantify what constituted "TMJ, or what quantified the pain in any of the four groups. By study design, more than 2/3rds of the total recording duration was performed at rest, and the raw data was heavily weighted toward rest scores. Group 4 (TMJ and bruxing problems) statistically declined from 13.57 (+/- 7.1) µV to a final level of 4.8 (+/- 2.4 µV), while group 4’s standard deviation also narrowed. However, this reported finding does not support the PAM as pain was present in the presence of hyperactive muscles, not hypoactive.
Molin28 tested equal numbers of controls against patients with mandibular pain dysfunction syndrome. A force transducer was placed in between occluding teeth, while the subjects clenched to obtained bite forces measured in Kiloponds (KP; 1 kilopond = 1 kilogram or 9.80665 Newtons). However no EMG recordings were made to evaluate subject muscle physiology. Because of the glaring “apples to oranges” comparison in their units of measure, kiloponds of force instead of microvolts for muscle EMG, this study cannot be used to correlate muscle physiology and pain in either PAM or VCT.
From Table 3 of Lund et al. entitled, “Summary of studies in which the amplitudes or areas of antagonist muscle EMG activity from subjects suffering with chronic musculo-skeletal pain, measured during the burst of the agonist muscle, were compared with control data.” The three TMD studies listed Moller et al 1984, Stohler et al 1985, and Stolher et al 1988 are also examined and conclusions discussed.
To clarify this Table’s title, Lund’s theory states that agonist muscles are relaxing (or at least lengthening) as the antagonist muscles contract. In mastication, the agonists are the temporalis, masseter and medial pterygoid, and the antagonists are primarily the lateral pterygoid and digastric muscles. This being the case Moller et al 1984, Stohler et al 1985, and Stohler et al 1988, should have measured (but didn’t) the lateral pterygoid and digastric muscles activity while the temporalis, masseter and medial pterygoid demonstrated closing bursts. Also, it would have been prudent to measure temporalis, masseter and medial pterygoid muscle activity during the opening burst of the lateral pterygoid and digastric muscles. Lund’s table that included these citations could possibly remain current depending on what point within the mastication cycle was of interest to study. One caveat; it is widely accepted that surface EMG cannot measure lateral pterygoid electrical activity, being deep muscles. And needle EMG cannot provide accurate recordings during mandibular movement because the movements alter needle position, producing artifacts. Importantly, none of the TMD papers discussed in this section performed antagonist EMG measurements to support Lund’s theory.
Sheikholeslam, Möller, and Lous29 examined 37 patients with functional disorders before and after “conventional therapy.” They were compared against 43 control subjects under mastication conditions where subjects chewed an apple for 30 strokes while having EMG recordings completed of the masseters and temporalis. Conventional therapy as it turns out involved splint therapy and occlusal corrections where “occlusal adjustment was the sole treatment used in 20 patients.” The paper does not specify the actual occlusal corrections made i.e., Cr-CO, or working and/or non-working interference removal. However, the authors stated, “on average, occlusal adjustment resulted in a reduction of postural activity, and of symptoms and signs in all muscles under study.”33
Unfortunately, their results do not support PAM but do directly support VCT, as the agonist muscles went from a heightened level of activity to a reduced level of activity. This was the single available study where EMG levels of masseters and temporalis were measured, then a treatment was rendered, after which participants were remeasured to observe post treatment changes in the muscle physiology. This study’s findings oppose the PAM as the patients had muscle quantitative estimates of “hyperactivity” over the controls and occlusal adjustments brought about relief of pain and post therapy EMG levels more consistent with controls.
An article by Stohler, Yamada, Ash30 published in-house by the University of Zurich was not made available to the public but appeared in a PubMed search without its’ Abstract. Neither the journal issue itself, nor any archived version of the study could be found. Further, the full paper was not located on Google Scholar or ResearchGate, making it impossible to determine any conclusions with respect to PAM or VCT? Even though the PAM literature cites it, the authors were unable to include it in this analysis.
Stohler, Ashton-Miller, Carlson31 examined mastication EMG data by under-sampling only 12 controls and 12 subjects with painful TMD. The authors failed to clarify which of the 40 different TMDs diagnoses were included. They reported between the two groups, there was no change in temporalis and masseter EMG means when subjects closed through the bolus. However, during the opening movement compared to the controls, the pain group had significantly higher EMG levels across all the elevator muscles. Sustained muscle spasm patients usually exhibit elevated resting muscle activity during a period without function when the muscles are theoretically relaxed. While no significant differences in EMG levels were observed in both groups when closing through a bolus, this finding hardly supports either VCT or PAM because there was no recorded hyper or hypo activity in the muscles of either test group. Whereas, sustained elevated muscle hyperactivity when there should be relaxation does favor the VCT rather than PAM because muscle hypercontraction is sustained.
Rugh and Montgomery32 evaluated 23 TMD pain patients and 23 matched controls using solely masseter EMG data. A 10-minute baseline recording of all participants was performed while subjects sat in a chair as still as possible. Then subjects were given a metal box that had a row of six red LED lights to hold in their lap. When the lights would randomly blink, the subjects were asked to depress the corresponding switch to turn off the blinking light, trying to make as few switch choice errors as possible, all while masseter EMG recordings were made. The authors reported that the TMD pain patient group had elevated baseline EMG levels compared to the controls, which modestly supports VCT. However, the pairwise mean EMG readings made during the light switch testing were not significant (initial EMG = 4.0µV; final EMG = 3.5 µV). No treatment was rendered and no pre and post EMG exist. This study’s findings do not support PAM, but the lack of masseter EMG change suggests that the stressful light switch game did not increase EMG levels, which does not support what the biopsychosocial theory proposes.
This was an inconsistent assortment of non-supportive PAM Literature. This does not impugn the work of the authors that Lund cited to support his model. But it does reveal that the literature, specifically in the TMD section of the PAM model, fails to support Lund’s concepts. The pain adaptation model is only a “hypothesis,” which the authors clearly state as fact in their first sentence. Lund and colleagues measured nothing, presented no original data, rendered no treatment under experimental conditions and presented no pre or post therapy EMG results. Instead, they adopted what others had studied, very similar to how biased literature is selected within a systematic review. It is an important point of the authors’ conclusions that of the five musculoskeletal conditions described, the one exception to all others was the condition of the facial muscles where muscles can behave hyperactive and not hypoactive (p. 685).24 An astute reader must question that conclusion, in light of the literature the authors cited that minimally supports the PAM.
The original PAM article looked at the whole-body muscle behavior and pain effects, of which TMD was a small component. Since then, other authors have taken those broad conclusions and applied them to the very unique and specific subject of TMD pain,34–38 which was the noted exception! Others have published very similar conclusions, stating that the Pain Adaptation Model is “evidence based.”34,35,37,38 Glassman and Malizia wrote, “Lund demonstrated that interferences do not cause hyperactivity but result in hypoactivity.”34 This statement is not factually true in that Lund demonstrated nothing of that sort.
It has already been stated Lund et al performed no experimental treatments or evaluations. Sheikholeslam, Möller and Lous performed the one and only study where treatment removed interferences and EMG data was evaluated,29 which gave clear support to VCT and not to PAM. Those authors also cited Michelotti,35 where they claim the introduced “interferences did not cause increased symptoms.”34 This statement is false, as well. Michelotti did short-term, small alterations of the test subjects’ occlusions by applying 250 microns of gold foil to their first molars, stating, “the golden strip only interfered with maximum intercuspation (centric occlusion), and did not cause lateral or protrusive interferences, or a slide in centric.”35 It has been well established with consistent results that both working and non-working interferences are real etiologic factors.6–23 Michelotti reported exactly what would be expected over the 8 days of observation; there was zero causative effect for adding zero excursive interferences. Although it is a subtle difference, altering the centric occlusion does not equate to adding working, nonworking, or protrusive interferences. Thus, the publication’s title was misleading, which was not recognized by either the journal’s editor or the reviewers.
Murray and Peck authored a paper entitled “Orofacial Pain and Jaw Muscle Activity: A New Model,”36 using Lund’s model as their primary framework. The New Model suggested that pain resulted in a newly optimized motor unit recruitment strategy that represented an individual’s integrated motor response to the sensory-discriminative, motivational-affective, and/or cognitive-evaluative aspects of pain."36 Since this concept could not be measured or tested and strictly represented an unproven hypothesis, the 4 studies put forth as support in their Table 3 for this version of the PAM will be analyzed below.
These four studies are critical support of this newly proposed model, as they addressed pain’s effect on postural EMG activity. Sherman’s findings have already been discussed.27 Glaros et al.39 tested fifty-four myofascial pain patients compared with 54 matched controls. EMG recordings of frontalis, masseter and temporalis muscles were made with lips and teeth apart. The authors concluded the TMD patients showed greater EMG activity than did non-pain individuals on all sites tested, but the differences between the two groups were statistically significant for only three sites.39 They did not explain their conclusion that the statistically significant differences in EMG activity between the two groups were not clinically relevant. Again, all EMG recordings were obtained under relaxed conditions, with all EMG activity being found higher at all test sites in the TMD group with greater variability. Although no therapy of any kind was rendered, these results failed to support PAM, but they did provide some support for VCT because muscle postural activity was higher in pain patients than in non-pain controls at all six sites.
Gervais, Fitzsimmons, Thomas measured masseter and temporalis muscle resting EMG levels for six-to-eight-minutes from three subgroups: asymptomatic (N = 24), subclinical (N = 31); and TMD patients (N = 61).40 The authors reported, the TMD patient group had significantly greater resting muscle activity out of the three groups.40 These findings clearly support the VCT because the affected pain group had hyperactive postural activity. Lastly, Burdette and Gale recorded EMG activity on 37 pain patients and 23 controls.41 They reported “the mean EMG value of the pain patient group was significantly greater than that of the control group, t (58) = 7.05, p < 0.05.”41 Again, this finding is consistent with VCT and gives no support to the PAM because the pain group had higher rather than lower EMG findings compared to the non-pain controls.
A year later Peck, Murray, and Gerzina wrote another review paper in support of their Integrated Pain Adaptation Model, but provided no data to support their model.42 They maintained the PAM was evidence based, yet provided no evidence to support their claim. In fact, their 2007 paper provided a few references that actually supported the VCT.36
Hodges and Tucker wrote a review about a new theory, “that provides a range of testable hypotheses,” although they didn’t state or test any hypothesis, provide any data or report any observations.37 Early in this review the authors opined that “many observations were inconsistent” with the vicious cycle theory. However, the only citation was Lund’s original paper, which lacks any supportive evidence for the PAM.
Finally, Mense wrote another review paper38 that was consistent with all other previous reviews, in that it provided very little in the way of evidence or data. Instead, the author claimed that VCT “should now be considered obsolete.” Ultimately, the author added nothing concrete to clarify the VCT/PAM discussion, only some opinions.
It is important to understand that all the authors who have supported PAM shared three commonalities:
-
None performed experiments using EMG muscle activity levels.
-
None accurately reported their subjects’ TMD condition(s), nor described any observations that consistently supported their paradigm.
-
All developed strictly theoretical research that resulted in opinionated review papers and included inconsistent, non-supportive literature with low evidentiary value.
It has been an oversight that review papers proposing a PAM hypothesis have been reported as being “evidence” by multiple authors.34–38,42 They are not and do not represent evidence, but reflect only the authors’ opinions.
Fougeront’s and Fleiter’s review paper about Temporo-mandibular Disorder with comorbid neck pain, which included no measured physiologic data, opined that both PAM and VCT theories “would apply partly” to the current paradigm of musculoskeletal disorders’ pathophysiologic understanding.43 These are the first authors to suggest both paradigms may play a role within the scope of TMD.
One group attempting to support the PAM, experimentally induced muscle pain by injecting 5% saline solution into muscles they were observing.44 Although injecting a hypertonic saline solution into muscle is painful, it does not make the muscle hypertonic physiologically. This is important because “hypertonic” refers to muscle spasticity or increased contractility versus a normal muscle tonus. The authors assumed a muscle’s behavior would be identical in function and pathophysiologic response, as seen with a chronic or acute TMD patient, as it would be with a saline injection. Nothing in the literature confirms this to be true, such that these authors’ bold assumption should not be overlooked. Many things can be done to make a muscle hurt, but they may not necessarily be physiologically relevant. In fact, a Medline search revealed that the only indications for using saline injections are hyponatremia, volume restoration, brain injury45 and to minimize the risk of steroid-induced atrophy.46
The purpose of the present article is to show EMG data as evidence of these 2 competing theories, within the context of before and after treatment of 2 TMD patients. This is important because, to date, the literature review processes has failed to produce even a single published example of utilizing EMG data as means to credibly support the PAM.
A Case Example in support of the Vicious Cycle Theory
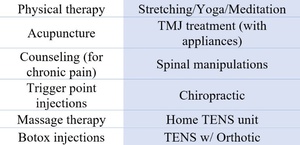
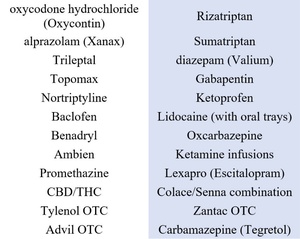
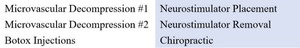
This 44-year-old female internal medicine doctor was diagnosed with migraines over 20 years ago and through those years, had no limitations of access health care. She completed orthodontics four times, each time trying to “get her bite right.” The first course was during high school, then later during her medical training and twice more after her training. She has seen over 37 providers, having tried a myriad of medications and therapies trying to address her migraines headaches. Figure 4. During consultation, she presented with an 11-page typed medical history and reported experiencing over 23 different symptoms, some of which were uncommon conditions. See Figures 5 & 6.
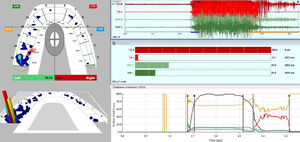
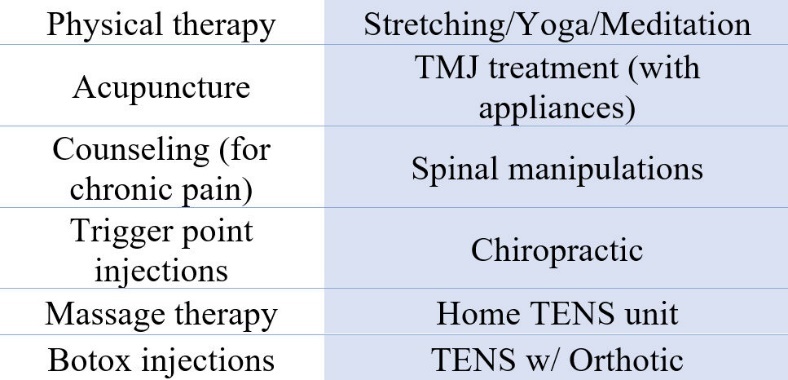
The patient reported most of her headaches were bilateral, but her migraines tended to be unilateral, affecting her left side with ongoing facial tension and ever-present pain. A digital occlusal analysis with the T-Scan10 synchronized in real-time to the BioEMG III electromyography technology detected 80.6% of the patient’s total bite force was on her left (affected) side. Figure 7. And bilaterally, both anterior temporalis muscles (in red) and both masseter muscles (in green) exhibited high and dense waveform amplitude (top right pane). The total of her first clench’s electrical activity reached 995.7 microvolts, indicating her four masticatory muscles were all hypertonic.
The same patient’s pre-DTR right lateral movement is visible in Figure 8. The Center of Force (COF) icon remains on the left side despite the patient moving right. Early in the excursion the left-side bite forces increase (from 80.6 % to 93.4 %) while the right-side forces decline (right = 6.6%), both resulted from the significant non-working interference that is frictionally shared between opposing contacting teeth numbers 15 - 18.
In this case, all pretreatment hyperactive muscles when treated occlusally with DTR therapy considerably relaxed, and painful headache symptoms disappeared lessening the patient’s required medication amounts, reporting, “I need those meds maybe 3 to 4 times a year as opposed to 3 to 5 times a week.” Figure 9.
A Case in Support of the (Theoretical) Pain Adaptation Model
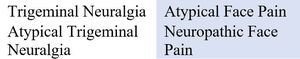
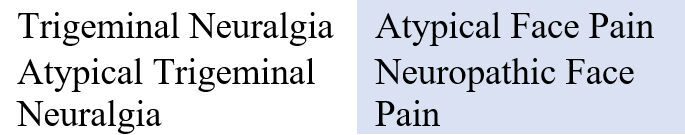
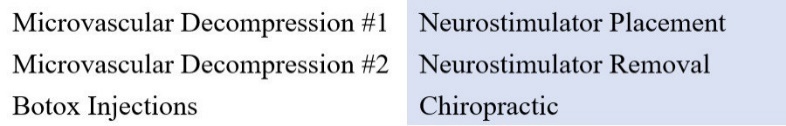
A 19-year-old female presented with unilateral left facial pain, that onset after a single dental visit when multiple fillings were completed in three quadrants of her mouth. She developed constant facial pain that sometimes-included electric shock sensations on the affected side. The unilateral pain intensified as more time passed. After several incorrect diagnoses, the patient was diagnosed with Trigeminal Neuralgia (TN), for which she consumed an extensive list of ineffective medications, and underwent six unsuccessful treatments (Figures 10, 11 and 12), attempting to relieve her TN pain. Her extensive symptoms at presentation are listed in Figure 13.
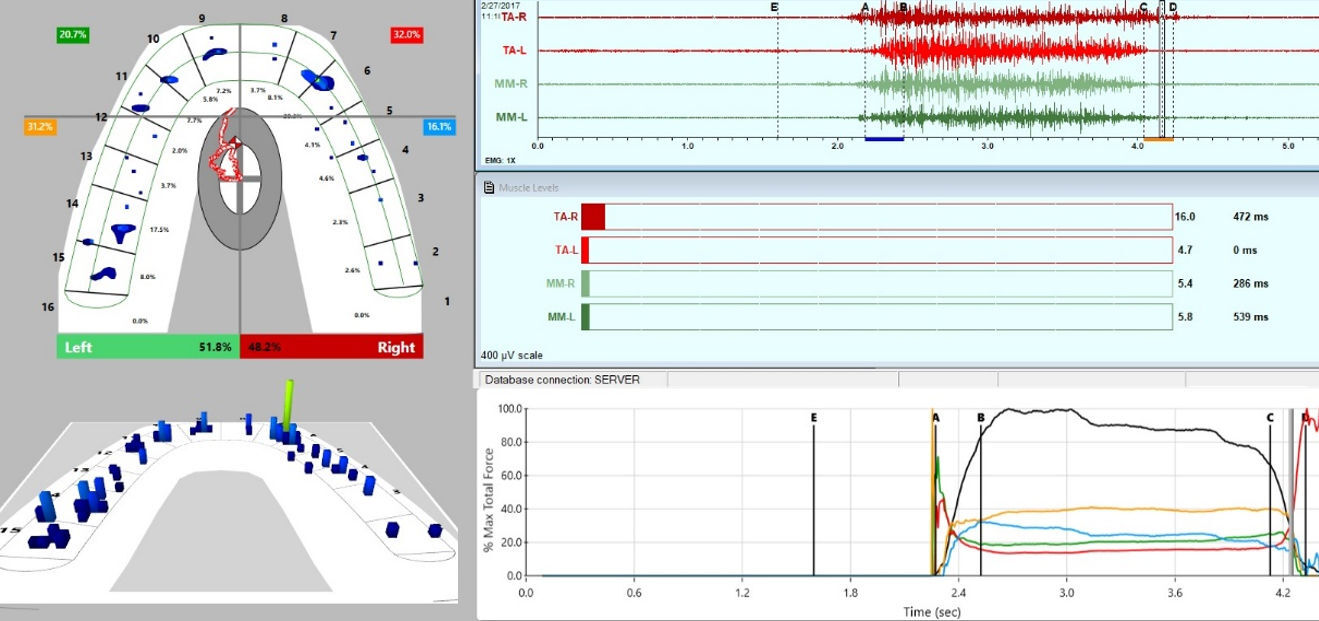
An occlusal evaluation with the T-Scan 10/BioEMG III revealed 62.7% of total bite force was on the left (affected) side, 37.3% was on the right side, with the patient visibly weak when clenching. During both MIP intercuspations, the muscles produced little electrical output. Figure 14.
After DTR was applied the muscle function was restored in the intercuspal clenching. Figures 14 & 15.
The observed improvements in muscle strength and contractility of case 2 are more consistent with PAM. This patient’s pretreatment 27 total symptoms were reduced to only two, the remaining lower back and shoulder pains required no medications of any kind whatsoever. Of course, an individual can suffer more than one painful condition simultaneously.
Discussion
Systematic reviews are held by many to be the pinnacle of scientific evidence. Figure 16.47 However, they do have the limitation of being heavily biased, as they are comprised of prior published articles by several of the authors48–57 that supposedly met their “inclusion criteria,” while many topic-related and useful articles are often excluded. Every systematic review is like a chain, in that it is only as strong as its weakest link.
The Lund et. al. systematic review discusses different aspects of human anatomy and muscle pathophysiology. By including animal models, describing elbows and other limbs, by explaining lower back pain, tension headaches, fibromyalgia, post exercise muscle soreness, as well as Temporomandibular Disorders, the article was intended to support the PAM. The title correctly indicates “…chronic musculoskeletal pain and motor activity.”24
The PAM authors state, “resting or postural muscle activity is no higher than normal in the five musculoskeletal pain conditions that we have described, with the occasional exception of the facial muscles.”24 A careful perusal of their supporting literature reveals this statement is a false conclusion. They theorize that the hyperactivity that is observed is unrelated to the pain and “simply a reflection of the changes in facial expression that pain often causes.”24 None of their supporting literature evaluated or measured facial expression.
Lund was a researcher and academician, but not a clinician. Four short years after proposing the PAM in 1991, he questioned the diagnostic validity of the monitoring tests used to diagnose Temporomandibular Disorders, one of which was EMG.58 He opined, “many tests lack theoretical validity, that measurement validity tends to be poor, and that diagnostic ability can be even worse than chance, because of the high percentage of false-positive diagnoses.”58 He further theorized that “this [EMG] may be very useful for research, but tests like this may not be appropriate for the clinic at this time.”58 These opinions required an explanation as to how using EMG or diagnostic technologies differed when diagnosing/treating patients or researching with patients. Lund offered none, such that his opinions regarding the of diagnostic value of physiologic technologies should be questioned. The author went on to further opine, “we suggest that, instead of concentrating on unproven devices and tests, prudent clinicians should recognize that the first aim of their therapy is to reduce pain, (even by non-specific means), and it is this variable that should first be measured.”58 To date there is no objective way to measure pain; it can only be subjectively assessed using a VAS scale or an ordinal number descriptive questionnaire. The diagnostic technologies Lund criticized provide objective, clinically-relevant, data via physiologic measurements, rather than unproven theories or conceptual prognostications.
This approach was not only ironic but short sighted, for if the PAM was to someday be proven correct, the purported changes in muscle physiology would require observation, measurement and verification using the same physiologic measurements obtained with the biometric technologies he criticized. Later he utilized that same EMG data to support the conclusion that masticatory efficacy of a long bar overdenture “was comparable to a fixed prosthesis.”59
A true scholar, upon realizing that their advocated beliefs might be fatally flawed, should seek to discuss the flaws that led to the “why,” to help further human physiologic knowledge. After all, there could be more than one possible physiologic explanation, despite someone advocating an “factual appearing” agenda or belief system. No one doubts that light behaves both like a wave and a particle.
This debate between VCT and PAM is a purely academic exercise that has no relevance when clinically treating patients. None of the PAM supportive literature offers new treatment options, or makes recommendations on how patients exhibiting TMD pain, signs or symptoms should be treated differently. Nor is there a decision tree of treatment recommendations based upon a patient’s muscle activity levels. Since no EMG was measured, the patients muscle activity levels can only be surmised as “hypo” or “hyperactive” being based upon the patients presenting (theoretical) painful symptom report. In stark contrast, the VCT literature is very consistent and specific, by using different biometric measurements to make the diagnosis and by guiding measurable treatment outcomes. The two presented patients were treated with the exact same therapy, Disclusion Time Reduction (DTR), via the Immediate Complete Anterior Guidance Development Coronoplasty (ICAGD),60 which has very well-defined, high-tolerance numerical occlusal adjustment endpoints that have been shown repeatedly to improve bite force profiles, contact timing, and muscle physiology.6–21,23
One interesting observation made during this literature review was that there is a very distinct “line in the sand” drawn whereby biopsychosocial proponents tend to support the PAM, while others that believe there is an occlusal etiology behind chronic masticatory muscle pain, tend to follow the VCT.
It is clear the PAM authors do not understand the significance of the hierarchy of scientific evidence. When there is not even one published case study, one animal trial, one cross sectional study, one case-control study, one cohort study or one randomized controlled study, performed by PAM authors, there is no supportive evidence to reach the highest level of scientific evidence within the hierarchy pyramid, the meta-analysis or the systematic review. PAM supporters have bypassed the building blocks that are comprise the pyramid’s foundation, potentially making any meta-analysis “a house of cards.” If we accept the pain model or theory that is “more evidence based,” dependent on the frequency it has been observed, measured and frequently re-measured, VCT is the overwhelming winner. Over the past 15 years, when diagnosing, treating and measuring muscle activity with EMG data from over 700 TMD patients, this author has observed that VCT was in play in patient improvements = 94% the time, no patient change = 6% of the time, with PAM accounting for less than 1% of TMD patient improvements.
Conclusion
It is a fool’s game to argue one theory is more accurate or evidence-based without actually measuring the patient’s physiology. Again, the discussion is purely academic, as successful treatment of these TMD patients was never predetermined based on each person’s initial muscle physiology as both example cases were treated with DTR via ICAGD.
The phrase “evidence-based dentistry,” (borrowed out-of-hand from evidence-based medicine), is used everywhere in the dental profession, yet appears to mean very little in the disciplines of TMD and Occlusion. This is however changing, as more providers are incorporating biometric technologies like T-Scan and BioEMG III into their clinical practices. Dentistry is slowly realizing the value of employing objective data for diagnosis and treatment planning, and to guide treatment parametrically, as well as to follow up and maintain physiologic health.61 Relying solely on subjective visual inspection or muscle palpation to analyze the complexities of the occlusion’s impact on the masticatory muscle physiology, is a limiting paradigm. To be fair to both Lund and coauthors, much more is known and understood now compared to the early 1990s, because of the increased implementation of diagnostic biometric technologies. Lund was correct in his description of muscle physiology under the PAM, but not because of any specific clinical observation, nor from outcome data generated during treatment(s), nor because the literature supported the theoretical model.
Science is a tool that can be manipulated and corrupted. Scientific integrity is limited by the integrity of the people performing the science, and their integrity in reporting accurate findings despite their beliefs, to avoid misleading the profession. Both VCT and PAM are explanations of how muscles may behave within the Stomatognathic system, and both presented clinical cases illustrated that differing physiologic changes from a single treatment can exist in nature. Therefore, great care must be taken to not globally advocate that a tiny sliver of theoretical literature (these biopsychosocial systematic reviews), be a widely accepted, universal, physiologic explanation, when it is clearly unproven and has minimal scientific foundation.
Conflict of Interest Statement
The 1st author (BS) is not a consultant to any dental materials or technology companies and has no financial interests in either. The 2nd author (JR) is Chairman of the Board of BioResearch Associates.







__with_the_r.jpg)











__with_the_r.jpg)

