Introduction
The Joint Vibration Analysis (JVA) system records and analyses the vibrations resulting from internal temporomandibular joint (TMJ) anomalies. It uses accelerometers to accurately measure the amplitude and the frequencies of vibrations emitted from the TMJ’s condyle/disc assembly during cyclic mandibular maximal opening and closing.1 Figure 1 illustrates the JVA technology placed on a patient’s head as it is recording vibrations. JVA correlates with disease state existence 75-94% of the time, (sensitivity), and does not indicate a disease state when there is no disease present 98% of the time, (specificity).2,3 Due to its high specificity, JVA is an excellent screening tool for TMJ internal derangements that assists clinicians in determining if a patient possesses normal or well adapted and stable TM joints. JVA can also be combined with MRI and CBCT to complete a detailed joint structural evaluation before any occlusal therapy is instituted. Most importantly, detected vibrations can reveal TM joint structural deformities because the differences in a vibration’s intensity and frequency content correlate to temporomandibular joint specific structural pathologies.4–10 The amplitude of a given vibration and its waveform pattern indicate the energy associated with a particular internal TM joint dysfunctional event.11 The amount of energy is combined with the frequency content, the range of motion, the location at which the vibration occurs along the patient’s opening or closing pathway, to indicate the most likely stage of disease progression according to the Piper Classification System.12
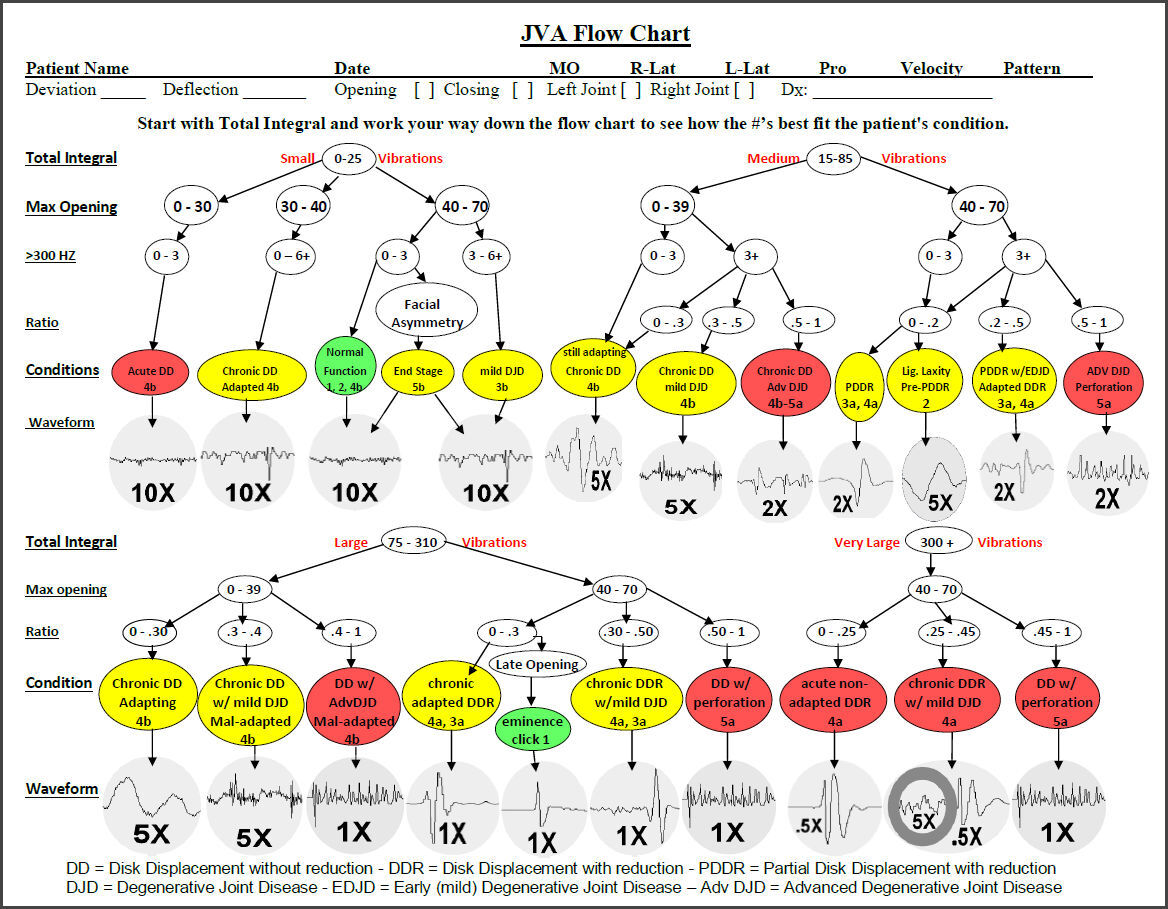
The JVA “Total Integral” integrates the amplitude at each frequency over the entire bandwidth into one number that is analogous to the relative amount of energy in a given waveform. It is the best indicator of overall intensity of a joint sound. It is subsequently divided into 4 parts, small , medium, large and very large intensity in the JVA Flow Chart (See Appendix). The frequency 300 Hertz is used as a reference because the frequencies below 300 Hertz are mostly due to soft-tissue initiated vibrations such as disk displacements and reductions, while those above 300 Hz are more likely due to harder-tissue initiated vibrations appearing only after degenerative changes have occurred within the TMJ.
The basic elements of JVA include measuring the overall intensity of each vibration (Total Integral) and calculating the distribution of vibration frequencies with respect to the reference frequency 300 Hz (< 300 Hz integral, > 300 Hz Integral) from both symptomatic and asymptomatic subjects.5–8 When the ratio of these integrals, (> 300 Hz / < 300 Hz), exceeds 0.3 substantial degenerative disease is present. Correlations have been made between the TMJ vibration characteristics and radiographs, with MRIs as well as with open surgical findings.7–16 The diagnostic accuracy of JVA has also been demonstrated.2,3,8,11,17,18
When the vibration data are combined with the range of motion (ROM) and with the patient’s signs and symptoms a reliable understanding of the current condition of each TMJ is possible.19 When the JVA indicates pathology, it can often suggest whether MRI or CBCT will contribute more information by qualifying the degree of degeneration.14 JVA has been used to evaluate the benefits of treatment20–24 and compared to other measurement devices.25 In one recent study it was concluded that: “The average Total Integral of TMJ vibration decreased significantly with the increasingly pathological state of articular disc,”26 suggesting it is a potential parameter related to chronicity. JVA has more than 30 years of research behind it ranging from comparisons to MRI, comparisons to CBCT and comparisons to surgical findings. It is a 3-minute procedure and can easily be assigned to the staff in a busy dental practice.
Patients with TMDs exhibiting symptoms of limited muscular pains often benefit greatly from Immediate Complete Anterior Guidance Development (ICAGD) coronoplasty.27–30 This procedure is also referred to as Disclusion Time Reduction (DTR) therapy because the procedure uses the disclusion time in lateral excursions as the best indicator of the presence of posterior occlusal interferences to function. This procedure is not chosen when the majority of a patient’s TMD symptoms are located clearly within the temporomandibular joints (TMJs) and the occlusion in not the primary cause of the patient’s condition.
Chronic Occluso-Muscle Disorder (OMD) is a subset of painful Temporomandibular Disorders (TMD) with painful symptoms primarily afflicting the masticatory musculature, whereby the lateral pterygoid is often affected.31–33
Chronic facial pain, temporal headaches, clenching, and grinding of the teeth, morning jaw pain, eye strain, earaches, tooth pain and temperature sensitive teeth, are all commonly reported dysfunctional symptoms.34–36 Patients that are suffering from a masticatory muscle disorder exhibit increased tonicity of the elevator muscles, creating an increased intra-articular pressure in the TM joint. Multiple published studies using the T-Scan computerized occlusal system have shown that muscular symptoms can be resolved with ICAGD.34–45
Objectives
Demonstrate the changes in TMJ vibrations resulting after DTR treatment of muscularly symptomatic TMD subjects. The null hypothesis was no change.
Methods
Inclusion criteria:
-
Patients having muscular TMD with minimal internal derangements diagnosed with JVA.
-
Patients having Class 1 (Angle’s Classification) or nearly canine coupling.
Exclusion criteria:
-
Primary TMJ internal derangements like closed locking, painful disc displacement with or without reduction, condylar avascular necrosis, loss of condylar height, a present tumor within the TMJ, markedly reduced vertical opening or super-erupted and/or mal-positioned 3rd molars.
-
Anterior open-bite occlusion patients were also excluded because not only could they not undergo ICAGD due to an absence of coupled anterior teeth, but MRI has determined that open-bite occlusion patients often present with serious soft tissue disc displacement events and degenerative TMJ structures.
-
Any subjects that were acceptable, but did not choose to participate.
Patients presenting in two separate dental practices of two highly trained ICAGD providers, well calibrated to use T-Scan for ICAGD, all demonstrated and reported limited joint noises and chronic painful muscular TMD-like symptoms and were recruited for participation. Potential subjects completed a medical history and a symptom evaluation questionnaire that was used to screen patients for possible study eligibility. Many of the selected subjects had previously experienced splint therapy, OTC pain medications, soft food diets or physical therapy.
Sixty youthful subjects suffering from primary muscular orofacial pain were recruited and agreed to participate (44 F, 16 M) from a student group with a mean age of 21.1 (+/- 1.85) years and an age range of 18 to 24 years. Patient questionnaires surveyed; 1) the frequency of ten painful symptoms (0 = never, 1 = occasionally, 2 = often, 3 = always), 2) the Beck Depression Inventory – II scores and 3) the PHQ-15 used for the evaluation of Somatic Symptom Disorders. Each patient was examined clinically and the T-Scan 10 was used to record their left and right lateral excursive disclusion times (Tekscan, Inc. South Boston, MA USA). This was done together with the BioEMG III (Bioresearch Associates, Inc. Milwaukee, WI USA) to simultaneously record the masseter and anterior temporalis muscle activity associated with the lateral excursive movements. A focus of this study was to record Joint Vibration Analysis (JVA) from all subjects using the BioJVA System (BioResearch Associates, Inc. Milwaukee, WI USA) that objectively detects the extent of any TMJ dysfunction prior to DTR treatment and then to re-assess each subject post-treatment. Subjective data were analyzed with Wilcoxon Signed-Rank test, measured data using Student’s paired t test. Figures 2 & 3.
The JVA recording requires the subject to follow a metronome in opening and closing to allow the system to estimate the position of the jaw at the onset of a vibration, whether during opening or during closing. The record includes six complete open to maximum and close to occlusion cycles, which forces both condyles to extend to their maximum anterior position and return to their centric occlusion position. See Figure 2. The post treatment example record is illustrated below in the Figure 3.
After being fully informed of the benefits and risks involved, those patients who consented were provided treatment in the form of Immediate Complete Anterior Guidance Development (ICAGD), which is also referred to as Disclusion Time Reduction (DTR) therapy because the goal of treatment is to remove posterior occlusal interferences to lateral excursions. The end point of DTR is indicated when the time required to produce the left and right lateral excursions is reduced to less than 0.5 seconds, the disclusion is produced with the anterior teeth and the muscle activity involved is reduced to a minimum. An example of a patient’s pre-treatment disclusion time is shown in Figure 4 and the same patient’s post-treatment disclusion time one day later in Figure 5.
Prior to any treatment this group’s substantial painful symptoms were surveyed (Table 1) and each subject also completed the Beck Depression Inventory – II prior to any physical treatment (Table 2).29 The pre-treatment BDI-II median score (24) suggests that the group as a whole was experiencing a moderate level of depression. Although it is not reliable to arrive at a diagnosis of Somatic Symptom Disorder (SSD) in the presence of physically painful conditions, some recommend evaluating a TMD patient during the diagnostic workup, even prior to any physical treatment. The problem with this approach is that the symptoms associated with SSD are the same symptoms that are also associated with physically induced pain. However, if after the treatment has concluded the patient still scores high on the PHQ-15, then an SSD diagnosis could be present.46–48 One caveat is that symptoms often retreat gradually in response to any treatment. Thus, some time may be required (1 week to several months) before a particular patients’ full recovery can be effectively assessed.
Results
of motion that were recorded during the clinical examination were compared to the vibrations and range of motion recorded after completion of the DTR treatment. The vibrations from the left TMJ decreased significantly in the intensity of the integrals (p < 0.05) and with a trend in the peak amplitude (p < 0.063). The same sets of measurements and analyses were made with respect to the right temporomandibular joints and found to be very similar. The ROM increased very significantly (p < 0.00000). Tables 1 & 2.
Pain Scores
A dramatically significant reduction in the pain scores was reported by the subjects one week after DTR treatment. See Table 3. Note: A score of 90 would be equivalent to a score of 50 on a 100 mm Visual Analog Scale. While these subjects were not severe cases probably due to the relative youthful status, the reductions were all highly significant.
The Beck Depression Inventory – II has been recommended as a means of evaluating the level of depression of all TMD subjects and is something of a standardized approach. While the pre-treatment median score of 24 suggested that the average subject within the group was suffering a moderate level of depression, one week post treatment the BDI-II median score dropped to 4, that was within the normal range of 0 to 10. No subject remained above 10 after treatment. See Table 4.
Perhaps due to the youthfulness of this group the mean PHQ-15 score pre-treatment was only 6.82. 54 subjects scored between 5 and 9, which might have been misconstrued as low SSD severity. Only one subject scored in the medium SSD range (10 – 14) and five scored within the normal range of 0 – 4. See Table 5.
The disclusion times were recorded prior to any treatment being rendered as part of the diagnostic work-up. A pre-treatment long disclusion time suggested a probable posterior occlusal interference condition. A short disclusion time post-treatment was considered as an indication of free entry into centric occlusion without substantial posterior occlusal interferences. Based upon previous mastication studies, the lateral excursive pathway is also normally used as the path of closure during unilateral mastication.49,50 The dramatic reductions in disclusion times as seen in this study are common after DTR therapy as that is the focus of the procedure. See Table 6.
During the recordings of disclusion times with T-Scan the activities of the masseter and anterior temporalis muscles were also recorded at “C” just before the excursion begins. This activity is produced in the intercuspal position so any increase in activity and balance reflects positively on the stability of the intercuspal position. The values increased prior to the right excursion (TA-R & MM-L) and exhibited a trend in the same direction prior to the left excursions (TA-L & MM-R). See Table 7. It was also determined that the EMG activity levels at “C” were significantly higher post-DTR for this group (comparing the mean values of the four muscles using the non-parametric Sign Test; p = 0.01267) than prior to DTR. A smaller standard deviation was also calculated indicating increased consistency in centric occlusion as well. See Table 8.
Discussion
Within this group of subjects the mean Total Integral (intensity at all frequencies combined) indicated that the group as a whole was characterized by a medium level of vibration (Total Integral = 24.1 on the left and 26.2 on the right) prior to treatment. See JVA Flow Chart in the appendix. Post treatment the group mean Total Integral was reduced to the level of small vibrations (15.5 on the left and 16.7 on the right); “small” also being the range of Total Integral intensity that is present within a control group of asymptomatic subjects.10 These subjects were screened with JVA to avoid any subjects with severe TMJ conditions that were not well adapted. See the appendix for the JVA Flow Chart.
The example JVA data in Figures 1 & 2 are typical vibration levels for muscular TMD subjects without substantial TMJ involvement, indicating a moderate (medium in the JVA Flow Chart) or low levels of vibration. The right opening vibrations were suggestive of a partial disk displacement with reduction. The vibration reduction together with no loss of ROM seen post treatment suggests that either the right TMJ partially displaced disk was recaptured (Piper 2) or the disk permanently partially displaced (Piper 3b). Neither of these conditions is serious. The vibration levels in the left TMJ were within the normal range (Total Integral < 20) both pre and post treatment. The small increase in the ROM was probably due to muscle relaxation.
The fact that the increase in the mean ROM distance was only 5.4 mm, but very highly significant, was due to the fact that not only was the mean ROM improved, but 55 of 60 subjects experienced at least a small increase in ROM, in many cases possibly just due to some muscle relaxation. Of the 11 subjects with limited ROM prior to treatment, only 3 remained so after treatment. See Tables 1 & 2.
TMD patients with primarily painful muscular symptoms, sometimes referred to as myofascial pain dysfunction syndrome (MPDS), are commonly thought to have a “muscle problem.” However, painful muscles can be secondary to malocclusion that causes excessive effort on the part of the muscles. The best evidence to support this in the literature is in the form of successful treatment with Immediate Complete Anterior Guidance Development (ICAGD) coronoplasty, also referred to as Disclusion Time Reduction (DTR).27–30,34–45,49,50 One limitation is the presence of chronic, poorly-adapted internal derangements of the TMJ. An internal derangement, with or without degeneration, can distort the structure of the masticatory system to the point that the arches are so mal-occluded, it is not possible to adjust the occlusion enough to correct the maxillo-mandibular mal-relationship. Thus, when selecting a potential patient for DTR therapy, it is incumbent upon the practitioner to evaluate whether TMJ function is sufficiently normal or well adaptated.30,46,47,49,50
According to the Beck Depression Inventory – II scores, this group was moderately depressed (median score = 24) prior to any DTR treatment. Post-treatment the median score dropped to 4, well within the normal range (0 – 10), indicating the previous real level of depression was related to their malocclusions and relieved after DTR in this group. See Table 4. Although it can be useful to understand the level of depression of each TMD patient prior to treatment, it is more important to understand that physically induced pain inevitably leads to some level of depression, especially when the pain is chronic, long lasting and seemingly without hope of resolution.51 To confirm that a patient’s level of depression is etiologically related to emotional factors, which can be the case, all physical etiologies must be removed from contention.
The Patient Health Questionnaire -15 (PHQ-15) is a validated instrument to evaluate a patient for a Somatic Symptom Disorder. According to their scores, 54 out of 60 in this group prior to treatment could have been labeled as mild SSD (scores between 5 and 9) and one as a moderate SSD (> 10). The other five scored within the normal range (0 – 4). Post ICAGD only five subjects remained within the mild SD range (5 – 9), none exceeded 9 and the rest (55) were all back into the normal range (0 – 4). Thus instead of evaluating 55 subjects for SSD, only 5 needed to be followed-up with a re-test at a later date.
For the PHQ-15 to be accurate patients cannot have any physical medical condition etiologically related to their painful complaints. The dramatic reductions in pains outside of the masticatory system in this group of young subjects reveals the whole-body effects that are possible with malocclusion. An 84 % reduction in stomach pain could be attributed to poor mastication and overall tiredness resulting from poor nutrition, but a 90 % reduction in back pain seems to be a rather distant connection. Tinnitus on the other hand has been associated with TMD in numerous previous studies.52–55 Thus, a 90 % reduction in tinnitus is not very surprising. An 81 % reduction in headaches for the group is also not surprising because headaches are probably the most common complaint from TMD patients.56
When applying ICAGD to shorten the disclusion time the subject bites down on the T-Scan wafer first and then makes a lateral excursion. Posterior occlusal contacts add friction to the process and slow down the progress. Removing posterior interfering contacts and creating anterior disclusion reduces the friction and speeds up the process measurably. While reducing the disclusion time is the goal of the process, the removal of the functionally interfering contacts is the benefit to the patient. This has been demonstrated previously in studies that have evaluated masticatory functional movements and simultaneous muscle activities pre and post ICAGD.29,49,50 In this study the EMG was used primarily to evaluate the reduction in activity between “C” and “D” during the lateral excursive movements because a lack of posterior contact automatically reduces the elevating activity of the masseter and anterior temporalis muscles. The level at “C” can indicate the degree of stability and the balance of the elevator muscles in centric occlusion as well. In this study the levels at “C” increased post ICAGD, but more importantly they became more uniform and less variable between the elevator muscles suggesting improved stability and consistency. See Table 8.
Conclusions
The intensities of TMJ vibrations recorded with Joint Vibration Analysis were significantly reduced post ICAGD as were the symptoms of depression that are very often associated with TMD patients. Somatic-like Symptoms, present with this TMD group pre-treatment, were fully relieved post-treatment. Along with muscular pain relief, after disclusion times were reduced, the muscle activity was observed to become more closely balanced.
Funding Statement
This study was not funded.
Conflict Statement
John Radke is the Chairman of the Board and Greg Kamyszek is the President of BioResearch Associates, Inc. No other potential conflicts of interest were present.

_late_opening_vibra.jpg)
._although_vibrati.jpg)
_and_very_hyperactive_right_anterior_temporalis_muscle_.jpg)
_and_much_lower_activity_of_the_right_anterior_tem.jpg)

_late_opening_vibra.jpg)
._although_vibrati.jpg)
_and_very_hyperactive_right_anterior_temporalis_muscle_.jpg)
_and_much_lower_activity_of_the_right_anterior_tem.jpg)