INTRODUCTION
People across the world suffer from temporomandibular disorders (TMD). The TMD patients present with a group of symptoms such as pains in the head and neck and clicking in temporomandibular joint, dysfunction associated with painful muscles of mastication and a limited range of mouth opening (ROM).1
In many individuals, TMD causes a severe masticatory functional disability. Significant research efforts have been invested in finding its etiologies. A number of etiologic factors are attributed to the onset of TMD. Its symptoms are significantly correlated to para-functional habits like bruxism, clenching and masticatory muscle tension.2
Many authors believe psychological3 and postural habits4 also influence the initiation of TMD. Other researchers have demonstrated there is a strong correlation between occlusal interferences and TMD, occlusal disturbances lead to orthopedic instability of TMJ and hyperactivity of the muscles of mastication eventually leading to TMD.5 Occlusal interferences that have been found to have an association with TMD are retruded condylar position (RCP) to intercuspal position (ICP) slide, balancing side, working side and posterior protrusive interferences.6,7 Patients with group function occlusion have been found to have more incidences of muscle hyperactivity than those with canine guided occlusion.8
The T-scan III occlusal imaging and analysis system could prove clinically useful as a diagnostic screening method for occlusal stability in the intercuspal position (ICP).9,10 A disharmony of the occlusal contacts in the ICP is, in fact, an important etiologic factor in TMD11 that cannot be detected, during the standard odontological evaluation.
Simultaneous bilateral contact time can be established using T-Scan III; (Tekscan Inc., Boston, MA, USA) since it measures the 1st contact to complete intercuspation.12 The computer-guided simultaneous contact ensures that no region of the dental arch contacts too early.13
Through this case report we intend to highlight the use of T-Scan and electromyography (BioEMG III, Bioresearch Associates, Inc. Milwaukee, WI, USA) in diagnosing and treating a case of TMD along with the presence of a vascular lesion, which until then was not detected.
CASE REPORT
A 23-year-old female patient visited the Dept. of Prosthodontics of Rajarajeswari Dental College and Hospital with a 2-year history of pain in her right temporo-mandibular joint, difficulty in left lateral movements, and difficulty in opening her jaw. She also complained of pain and difficulty in chewing hard food. The pain was intermittent, which mostly occurred during the morning hours. She was previously treated by a general physician and a general dentist who advised and extracted a third molar, but there was no reduction in the symptoms afterwards.
METHODS
On extra-oral examination there was facial asymmetry, a visible swelling on the right side of the face, which was not observed by the patient. On Intra-oral examination the patient had a canine-guided occlusion with bilaterally class 1 molar relation. On palpation of the muscles, the right lateral pterygoid and the right masseter muscles were tender. Note: As part of a routine treatment protocol for TMD cases, she had been treated with an occlusal splint by earlier dentist.
The patient was advised to stop all analgesic medication, to be on a soft diet and advised to
perform mouth exercises, so that her mouth opening would not decrease further. The patient was asked to use the splint throughout the day and report back after three weeks.
After three weeks, the patient reported back with the same symptoms, with no relief in pain although, the swelling had decreased since the first visit. A hard splint was fabricated and delivered to the patient on the same day. Tab. Tolpa D (Micro Labs, India, having Diclofenac 50mg and Serratio-peptidase 10 mg), a muscle relaxant, was advised twice daily. The patient discontinued wearing the occlusal splint, as appliance therapy had not appreciably reduced her symptoms although the swelling was reduced.
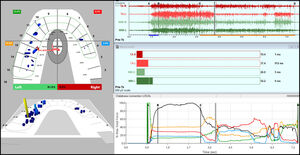
Then the patient underwent T-Scan III, BioEMG III and Joint Vibration Analysis (BioJVA: Bioresearch, Inc. Milwaukee, WI, USA) recordings to determine her occlusal function and masticatory muscular contraction patterns and the status of her TMJ. The patient was asked to bite hard into the sensor and open, for three times for a Multibite. Figure 1.
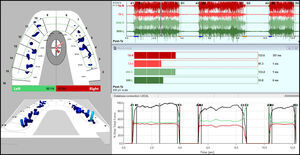
The patient was asked to bite hard and hold for few seconds and then to glide to the right or glide to the left to obtain the excursive records. See Figures 2 & 3.
RESULTS
The T-Scan III analysis pre-treatment showed long Occlusion Times (OT) for all three movements. Figures 1-3. The Disclusion Times (DT) for both left and right lateral excursive movements showed values of 4.17s and 2.45s respectively, which are indicative of functional occlusal interferences. These values were all outside of the known normal physiologic ranges: OT < 0.3 s; DT < 0.5 s).12,14 These are some major contributing factors for occluso-muscular painful symptoms in patients. The patient was instructed that her disclusion times were too long, causing excursive muscle hyperactivity detected in the EMG data, see Figures 2 and 3 to the right of line C, which it was anticipated caused her muscular symptoms. It was further explained to her that muscular pains could be minimized or eliminated if she elected to have her Disclusion Times Reduced (DTR) utilizing Immediate Complete Anterior Guidance Development (ICAGD) occlusal therapy.
The JVA assessment determined that the patient had no substantial internal derangements of any significance. See Figure 4.
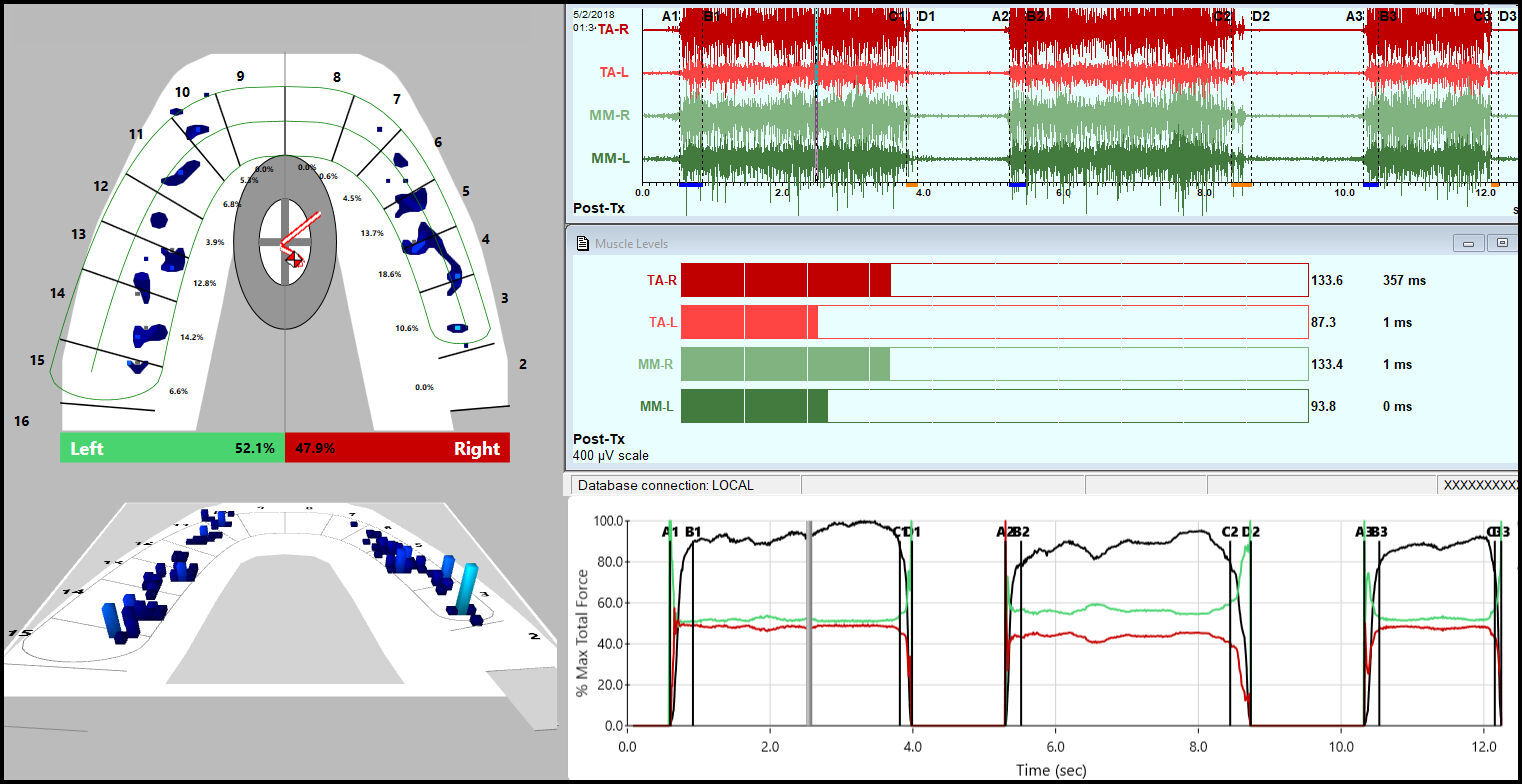
After obtaining the patient’s consent, ICAGD enameloplasty was performed using her right and left lateral excursive movements, reducing the prolonged occlusal surface friction, which then shortened the DTs to within physiologic limits. The T-Scan/EMG records were repeated after ICAGD to measure the post treatment occlusion and disclusion times. See Figures 5, 6 & 7.
The corrected OTs and the corrected DTs for both the left and right lateral excursions are shown in Figure 8 after the completed enameloplasties.
The DT for Left and Right excursive movements was reduced to 0.35s and 0.35s respectively. See Figure 8. Hence, DTR shortened the contraction times of the involved muscles, allowing the ischemic and deoxygenated painful muscle fibers to recover a more normal metabolism.15,16
After three sessions of T-Scan and EMG evaluation and occlusal corrections, the patient reported with decreased pain and headache, and decreased swelling. The patient had stopped all of her medications, improved her mouth opening and improved the lateral excursive movements.
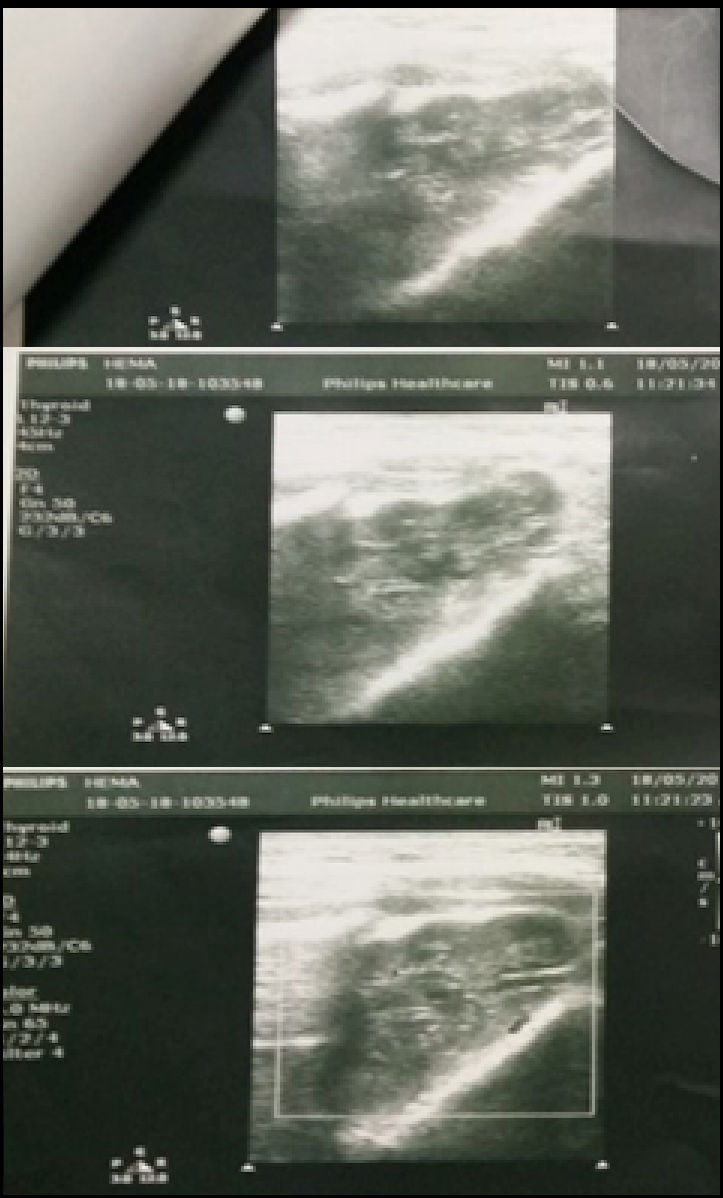
The patient was recalled after three weeks for a review. Patient returned back to the department after two more weeks and complained of slight pain once in a while. On examination, a diffused swelling and redness was seen anterior to the parotid gland of the right side. The patient was referred for ultrasound of the parotid gland and facial muscles.
The results of the ultrasound indicated a normal parotid gland, a bulky right masseter muscle and a small pocket of fluid collection, Figure 9. We referred patient for an MRI scan of the facial muscles, which in turn revealed the presence of a vascular lesion. So, drainage of the fluid was not carried out in this case, as it was a vascular lesion as per the MRI report. The patient was explained about the vascular lesion, which was the main cause for the recurring muscular symptoms even after DTR. It is important that we have a good understanding of these conditions so that the risk of potential complication of dental treatment in affected patients is reduced as much as possible. Significantly, it is not uncommon for a TMD patient to have more than one pathological condition.
DISCUSSION
The etiology of TMD is multifactorial, and all local, peripheral and central factors have sometimes been considered important.14,16,17 The present case report illustrates that secondary TMD symptoms of muscular pain respond well to occlusal adjustment therapy that is guided by occlusion and disclusion timing measurements. This type of patient’s response, has been reported in many published studies and clinical reports where the DTR therapy has been carried out for occluso-muscular TMD symptoms.13 Lengthy disclusion time has been shown in EMG studies to elevate excursive muscle activity levels, and efficient reduction of the disclusion time to less than half of one second can reduce the muscle hyperactivity and related painful symptoms.13 Properly performed, DTR represents a marked improvement in the treatment of myofascial pain dysfunction symptoms when compared to unmeasured occlusal equilibration involving centric relation manipulation and other commonly employed symptom-focused, non-occlusal therapies.13
Appropriate therapy can never be initiated unless a proper diagnosis is established. The clinician’s important task is detecting the type of occlusal parameter strongly correlated with TMD. Occlusal evaluation using digital methods in TMD patients will provide the accurate information about factors accountable for occlusal instability. Identifying the factors responsible will facilitate precise diagnosis and effective treatment.
Vascular anomalies constitute a diffuse group of conditions which can range in their significance from being completely harmless and of little clinical relevance to being potentially life threatening. Clinical development of the lesion is slow and painless; however, minor trauma can cause pronounced bleeding due to their highly vascular makeup. Although these lesions may affect all ages, they most commonly affect females in the second decade of life, possibly due to the vascular effects of female hormones. It is thought that poor oral hygiene, and localized factors such as improperly fitting restoration margins or calculus, can increase the likelihood of these lesions developing.18
CONCLUSION
After treating the patient using DTR therapy, this patient’s TMD symptoms have been resolved and she has been advised to come for regular reviews regarding the vascular lesion.
Funding Statement
No funding was received.
Conflict Statement
No Conflicts were reported.