INTRODUCTION
Dental Medicine has consistently employed traditional non-digital occlusal indicators to assess the force levels of occlusal contacts. The most widespread non-digital tool of Occlusion is Articulating Paper, which leaves ink marks of varying sizes and color intensities on contacting teeth. The prevailing theories suggest that articulating paper marks indicate occlusal contact force levels based on the mark’s size, shape, and color intensity. Several Occlusion texts advocate the known principles of Subjective Interpretation1–6:
-
Darker and larger paper marks indicate higher force contacts
-
Smaller and lighter paper marks indicate lighter forces contacts, and
-
The “Bullseye” contact mark results from high occlusal force levels removing some ink from the center of the contact mark.
The principles of Subjective Interpretation are still being taught as being safe for patients, despite that studies show dentists choose incorrectly both forceful and non-forceful contacts when using its’ principles of size predicting load.7,8 A 2007 showed that a large paper mark represented a forceful contact only 14% of the time, and another found that no correlation existed between mark size and applied occlusal load.9,10 In one cast and articulator study, it was reported that as applied occlusal forces were doubled and tripled, the paper mark sizes became smaller rather than doubled or tripled (which the “size of mark” theory would advocate).11 This finding occurred because higher forces chopped up the paper into small bits, such that the ink marks went down in size as the load went up.
What is well-known but has not been widely adopted, is that traditional static dental occlusal registration materials (foil, articulating paper/ribbon, ink impregnated strips, wax, or silicone imprints) do not quantify occlusal forces, detect occlusal contact time-sequencing, or detect force transmission around the dental arch.12,13 Articulating marks specifically, only indicate occlusal contact location; not occlusal force levels and contact timing durations.9,10 Most importantly, despite that it is still advocated that mark size describes occlusal force, no evidence exists illustrating articulation paper mark sizes accurately describe occlusal contact levels.9–15
Another important aspect to this ongoing paper mark size/lack of force level descriptive controversy, is that two separate studies illustrated when 400 subject-dentists chose force levels in 11 photographed quadrants of paper markings by visually assessing the markings, the subject-dentists chose correct forceful contacts only 12.8% -13.3% of the time7,8 while incorrectly Subjectively Interpreting the articulating paper markings 87.7% - 88.2% of the time. And, although articulating paper markings can be used with Shim-stock foil, Shim-stock also involves dentist subjectivity, to “judge” the resistance the foil exhibits from being removed.3 Ultimately, because Shim-stock does not mark occlusal contacts, articulating paper is used to identify forceful and non-forceful contacts.12,15
In contrast, multiple studies have validated the T-Scan sensor’s occlusal force reproduction and its timing quantification.14,16–22 Furthermore, both a reliable T-Scan recording method and definitive treatment protocols have been developed and tested in research environments, making it possible for dentists to use T-Scan data with dental patients predictably, and reliably.23–29 There are presently 5 published volumes that describe all of the researched T-Scan clinical applications in Dental Occlusal Diagnosis, Fixed and Removable Prosthodontics, Implant - supported Prosthodontics, Periodontics, Orthodontics, Aesthetic Dentistry, Cold Tooth Hypersensitivity, Temporomandibular Disorders, and Mandibular Orthosis for Body Posture and Balance.28
The T-Scan Novus HD recording sensor (Tekscan, Inc. S. Boston, MA USA) is a resistive, electronic tactile sensor that contains pressure-sensitive conductive ink distributed in columns and rows that are encased in Mylar, formed in the shape of a dental arch (Figure 1a and b).16 The HD recording sensor has been shown in studies to maintain its structural integrity for up to 24 crushes, and reproduce 256 occlusal force levels 95% of the time.16,18 In the 2 prior subjective Interpretation studies, the T-Scan detected the highest and lowest forces in the 11 different quadrant photographs that were used to test the clinicians (Figure 2) (a pink column denoted the highest force; a blue/black column denoted the lowest force).7,8
Surveys have been used in all forms of medicine and dentistry to assess a myriad of subjective perceptions about patient symptoms (frequencies and intensities),22,25 and as a measure of response to treatment.19,22–25 Surveys can also be used to gather demographic data for determining distributions of a populace being studied. Polling a Facebook group of dentists is a new form of surveying, where individual group members can respond to the question being asked, while the results of the entire groups’ responses can remain hidden from the group until the entire poll is completed.
The Specific Aims of this study were to replicate or contradict prior Subjective Interpretation study findings, by using T-Scan contact force levels in a single articulating paper-marked quadrant photograph, to see if a 3rd group of dentists-participants could visually select the 2 highest force occlusal contacts. A 2nd aim was to determine whether the group of participants agreed closely, or widely disagreed, about which were their perceived ink-marked, highest force occlusal contacts.
METHOD
A single maxillary quadrant occlusal photograph of teeth #s 11-17, was shot in a mirror after being fully marked with blue articulating paper, by a patient self-intercuspating into MIP three times, and holding their teeth momentarily clenched together between each intercuspation. From the ink markings left by the articulating paper, 9 distinct inked contact areas were circled and numbered to delineate the contact choices from which the dentist-participants would make their most forceful contact selections. Participants chose the number of each contact that was perceived as their two choices for the highest force occlusal contacts (Figure 3).
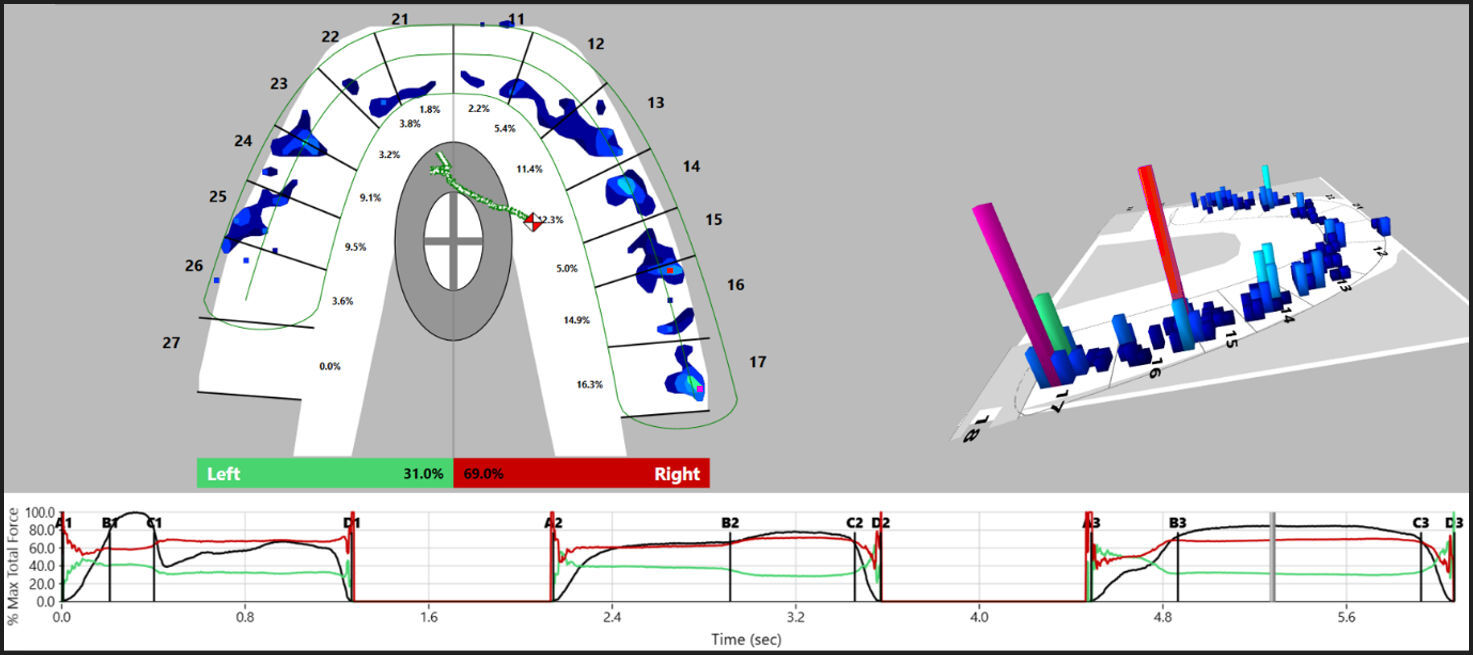
After the photographing was completed, the same patient made a 3 multi-bite closure T-Scan recording, by intercuspating 3 separate times into the HD T-Scan sensor firmly, and holding their intercuspation firmly clenched together between each intercuspation for 1-3 seconds, before opening and re-closing. The 2 highest force contacts isolated by the T-Scan were used as the answer key to compare to the dentists’ high force contact choices (Figure 4).
The single occlusal photograph was uploaded to a Group Facebook page that is comprised of 3633 Dentists. The member Dentists post topics of interest regarding general dental knowledge, clinical insights, research findings, and procedural descriptions, for comment from other member dentists. The only Inclusion Criteria were that the volunteer participants were members of the same Facebook group, and that they were Dentists. No demographic data was gathered, and no age limitation or years in clinical practice requirement existed to exclude dentist-participants. In this way, a broad range of fully blinded participants could respond to the post.
The single occlusal photograph post queried the entire Facebook group as to which of the nine contacts in the photograph were the 2 highest force contacts. 123 dentists participated in this blinded polling while the Facebook post remained available to the entire Facebook group. When no more dentists participated for 30 days running, the final percentages that each of the 9 contacts was selected as being the 2 most forceful contacts were tabulated and graphed (see Figure 6).
The dentist-participant choices were scored against the T-Scan data of contacts #s 4 and 9, as they were the 2 highest force contacts in the multi-bite recording using the Student’s t-test (Figure 5). The percentage selections made by the 123 dentists were statistically analyzed for their normal distribution using the Jarque-Bera test, and then compared for their choice agreement/ disagreement. (α = 0.05)
In addition, in order to evaluate the effect that “chance” had on the subjects choosing the correct contacts (as opposed to the effect from contact determination skills and acumen that a doctor uses), a randomized set of 123 integers limited to the range of one to nine (no zeros), was generated in an Excel worksheet (Microsoft Excel 2019; Microsoft Corp., Seattle WA, USA), for comparison against the subject groups’ 1st and 2nd set of contact selections.
RESULTS
From a total of 246 choices made, only 12 correct highest force contact selections were made (4.88 % correct; 95.22% incorrect). Only eight participants chose contact #4 as their first choice, and no participant chose #9 as the first choice. Two different participants chose contact #4 as their second choice; and two others chose contact #9 as their second choice. No participant chose both contact #4 and contact #9 (the two highest force contacts). Of the first contact choices, only 8 were correct (6.5 % correct; 93.5% incorrect), and of the second choices, 4 were correct (3.25 % correct; 96.75% incorrect).
Figure 6 shows the distribution of the 1st and 2nd high force contact choices made subjectively by the participants, with each contact’s bar matched in color to the T-Scan force level color describing the force level of each numbered contact.
Comparing the subject group performance against random contact selection chance, the mean value of the random set of chance contact selections was close to the mid-point, between 1 and 9 at 4.902 (+/- 2.627). However, the mean value of the participants’ first choices was 3.918 (+/- 1.952), which was significantly smaller (p < 0.0011) than random chance. The participants demonstrated a significant preference in their first choice for more of the contact numbers below 5, rather than the numbers above 5, and no participant selected contact #9 as their first choice. The mean value of their second choice of contacts was significantly higher than the random set at 6.33 (+/- 1.630). This indicates the participants showed a significant preference for choosing the numbered contacts numbered higher that 5 to be a valid “second choice” (p < 0.00001). No participant selected contact #1 as a second choice.
DISCUSSION
The findings of this study strongly indicate for the 3rd time, that dentists cannot accurately determine high occlusal force contacts by making subjective interpretation visual assessments of articulating paper mark size, color-depth, and shape. The results directly support the findings of the two previously published Subjective Interpretation studies.7,8 The reported low score of 4.88 % correct answers for the 123 dentist-participants is markedly lower than the findings of the 2 prior studies (12.8% and 13.13% correct contacts selected). This lower correct percentage seen in this study may have resulted from protocol differences. In this study, all participants observed 1 clinical photograph and were all choosing the highest force contacts from 1 set of articulating paper ink markings. But in the 2 prior studies, participants observed 11 totally different photographs of 11 different quadrants of articulating paper ink markings.
In Figure 6 (the Bar Graphs of the first and second choices), note that all the second choices were higher numbers than were the first choices. It appears that the participants started their observations at contact 1, proceeded to the first contact that “looked high”, proceeded to the second one that “looked high” and stopped analyzing, suggesting that dentists have a propensity to adjust the first ink mark that appears “high”, rather than observing all of the marks first. This is one possible explanation for why very few dentist-participants chose contact #9 correctly as being a high force contact. Most participants may have already chosen two marks before considering #9. This approach resulted in a lower percentage of correct choices than could have been accomplished by random chance. Most importantly, the very limited ability of the dentist-participants to choose the correct high force contacts, was in excellent agreement with the findings of both prior Subjective Interpretation studies.7,8
The fact that the participants scored only 12 correct answers total, being much less than pure chance (26 correct answers), differs from the scores observed in the 2 prior studies.7,8 In this study, the other correct high force contact #4, was also underrepresented at only 8 selections, versus 12 selections that could have occurred purely by chance. It would appear that whatever rules the participants used to select the high force contacts, led them astray.
When visually assessing the ink markings in Figure 3, the majority of first choices were contacts #s 1, 3, 5 & 6, which were rather evenly distributed. Something about those choices appeared to be commonly indicative of “high force” in the participant’s collective opinions. Contacts #s 3, 5, and 6 are the darkest and largest makings in the photograph, which suggests that these were favored selections because of the size of the marks and their dark color, which falsely indicated a “forceful” contact. It’s also possible that the most frequently selected contacts were favored because of where they were located on the teeth, such as being on an incline.
The majority of second choices high force contacts were limited to #s 6, 7 & 8, with #6 being the most frequently selected. When looking at contacts #s 4 and 9, they appear smallish and lighter than #s 1, 3, 5, 6, 7, and 8, but are actually high force contacts. Making these types of subjective visual assessments of the 6 most favored selections did not help the dentist-participants choose the correct contacts. One recent study concluded that, “…relying on articulation foils to evaluate occlusal contacts may still be viewed as the best available clinical method.”30 That absurd opinion does not survive when compared against this study’s scientific facts.
It is very concerning for the dental patients’ well-being, that to the majority of the participants 6 of the 9 contacts chosen appeared to be high force, which means that the group was not able to truly discriminate different force levels when looking at different paper makings. Carey, et. al, and Saad, et. al, found that small marks can often be high force contacts, and larger marks can often be low force contacts, and that as occlusal forces go up, mark size often goes down.9,10 So it was the long believed but (once again) disproven principle that large dark marks are forceful,1–6 that led the participants astray from finding the correct high force contacts.
Despite that studies have proven that the size and color depth of articulating paper do not accurately predict occlusal force levels,9–14 in this study and the 2 others that preceded it, low force contacts were chosen by clinicians as being high force, because they were the biggest inked areas on the occlusal surface. Of further concern is that these unfounded and non-scientific size and color depth guidelines of how dentists should use Subjective Interpretation principles. are still being taught in Dental Schools and Continuing Education Continuums, as if Subjective Interpretation is a safe and reliable method for dentists to utilize on patients. It is clear that Subjective Interpretation principles do not isolate the correct contacts, which does not bode well for patients and any occlusal treatment patients may undergo. Unfortunately, subjectively interpreting occlusal contacts actually puts patients at great occlusal risk
Alternatively, the T-Scan technology readily isolated the two most forceful contacts that the dentist-participants could not locate using articulating paper (Figures 4 and 5). The 2 pink columns visible in the 3D Force View window readily identify the correct high force contacts, while the 2D Force View window coordinates the high force contact to the tooth and contact location corresponding to the paper mark. This non-subjective method ensures that existing high force problematic contacts will be accurately located by the dentist. The T-Scan removes the subjectivity of looking at paper makings and replaces it with objective force and timing data sets that guide a clinician to make targeted and accurate occlusal corrections of the truly forceful contacts.
The patient clinical implications of selecting incorrect and unforceful contacts using unscientific subjective interpretation principles
The patient clinical implications of dentists choosing the wrong contacts are many31:
-
The removal of excessive tooth structure from areas of teeth that do not need occlusal force reduction, leading to possible weakened enamel and thinned enamel tooth sensitivity
-
The thinning out and weakening of occlusal dental materials present on various types of dental prostheses. This thinning and weakening could lead to early material failure and shorten the lifespan of the involved prosthesis
-
The potential for destabilizing a patient’s occlusal comfort level, leading to the appearance of occlusally activated tooth pain, and/or the sudden onset of previously absent TMD symptoms.
-
The potential for the clinician to not treat the true high force areas because the paper marks do not appear to the clinician to be “forceful looking”. This lack of excess force removal will lead to the ongoing existence of localized, occlusal force overload on some tooth contacts. Long-term, this could lead to tooth structure fracture, occlusal wear, tooth mobility, abfraction formation, gingival recession, periodontal bone loss, and peri-implant bone loss.
Because Subjective Interpretation is so prone to lead clinicians to make improper contact selections, it represents a maximally invasive treatment approach when performing occlusal adjustments. The insertion of an unbalanced occlusion may be the direct result of a dentist subjectively choosing the wrong contacts and adjusting the wrong contacts.31
LIMITATIONS
This study’s main limitation was that the picture of the ink markings was being observed without any patient feel input to help the clinician ascertain any areas of perceived contact “highness.” However, it was recently determined that patients were not as reliable about sensing occluding forces, as were the doctors in the same study who analyzed the patients’ occlusions.32 A second limitation was that none of the participants were able to examine the patient, which could have helped them better determine the correct high force contacts, and therefore might have improved their group score. And a third limitation may have been that the articulating paper marks in the quadrant picture were not made by the specific paper/ribbon type used clinically by some of the participants. Some of the participants may have been unfamiliar with the appearance characteristics of the photo-graphed ink markings, when they chose their perceived high force contacts.
CONCLUSIONS
Subjective Interpretation of articulating paper markings is a very inaccurate method of selecting forceful occlusal contacts for occlusal diagnosis and when performing occlusal adjustments. Visual assessments made of ink markings that do not measure occlusal force in any way are very unscientific, and can put patients at risk from poor contact selections made by a treating dentist. Due to its high rate of clinician error, subjective interpretation greatly increases the chances that low-force or moderate-fore contacts will be incorrectly chosen for treatment, while damaging high force contacts are unknowingly left in place. Replacing Subjective Interpretation with a measured contact force level detection method would be in the best interests of patients.
Conflict of Interest Statement
The Corresponding Author is a Consultant to Tekscan, Inc. and receives no monetary gain from sales.
Funding Statement
No funding was received from any source.