Introduction
Living with chronic pain is known to have significant, negative effects on a patient’s quality of life, in that declines in the emotional wellbeing of patients who live with chronic pain has been documented in the psychosocial dental literature.1 Temporomandibular Disorders (TMD) is comprised of numerous physical diagnoses including myalgia (muscular pain), that has been shown to have negative effects upon a suffering patients’ life quality.2 Studies indicate that regardless of the causative etiology, chronic masticatory muscle pain has been associated with negative emotional consequences.3–5
Some psychologists and psychiatrists have opined that TMD patients overreact emotionally to their chronic pain, suggesting that any physical dental or TM Joint structure breakdown, was secondary to anxiety, depression, and/or somatization.6 A psychological intervention with Cognitive Behavioral Therapy (CBT), has been recommended by some, to reduce a patient’s stress to (hopefully) reduce the TMD patient’s clenching and grinding habits, while improving their emotional outlook.7 However, 2 studies that compared “usual TMD treatment” combined with CBT and without CBT, showed CBT did not add a statistically significant treatment outcome contribution.8,9
Generally, medications and psychotherapy are employed for most patients who are experiencing depression. The commonly used medications are:
-
Selective serotonin reuptake inhibitors (SSRIs).
-
Serotonin-norepinephrine reuptake inhibitors (SNRIs).
-
Atypical antidepressants.
-
Tricyclic antidepressants.
-
Monoamine oxidase inhibitors (MAOIs).
Sometimes, combining two antidepressants, or adding medications like mood stabilizers, antipsychotics, anti-anxiety, and stimulant medications, may be recommended for a specific patient’s depressive state.
Although bite treatment is not a routinely recommended treatment for emotional depression, limited literature does exist where depression statistically improved after TMD patients underwent occlusal treatment to address their chronic pain state.10 Recently, 83 chronic pain patients were treated with the ICAGD coronoplasty (Immediate Complete Anterior Guidance Development),11 to shorten their Disclusion Times (DT), while the Beck Depression Inventory (BDI-II) reliably detected and scored the patients’ degrees of depression from pre to post ICAGD treatment.10–13 The BDI-II and the four additional pain and symptom questionnaires were filled out by each patient prior to ICAGD, 3 weeks later, and 3 months after ICAGD. The authors reported statistically significant reductions for the whole patient group in both pain levels and symptom frequency at 3 weeks (p < 0.00001), with further reductions after 3 months (p < 0.00001). Headaches were also less frequent at 3 weeks, and further improved at 3 months following ICAGD (p < 0.00001). And importantly, statistically significant reductions in the BDI-II scores were seen in all pre-treatment depressed patients both at 3 weeks and further at 3 months (p < 0.00001). The authors concluded that the dramatic reductions in BDI-II scores were resultant from the patients no longer living with daily painful physical symptoms.10
Occlusal interferences, prolonged Disclusion Time, and occlusal surface friction present during mandibular excursive movements are all etiologic factors for Occluso-muscular pain and symptoms observed commonly in TMD patients.14–18 The measurement-driven & computer-guided occlusal adjustment procedure known as ICAGD,11 measurably decreases the time required for all molars and premolars to disclude from each other (known as the Disclusion Time) in ≤ 0.4 seconds during right and left mandibular excursions commenced from complete intercuspation in Maximum Intercuspal Position (MIP).11 ICAGD has specific time-duration, numerical endpoints that must be achieved to verify the coronoplasty was properly accomplished.11,19 ICAGD is guided by the T-Scan 10 occlusal analysis system (Tekscan, Inc., S. Boston, MA, USA), that is synchronized with the BioEMG III Electromyography system (Bioresearch Assoc., Milwaukee, WI, USA).11,19 Together, they simultaneously record real-time force movies of mandibular excursive movements, and those same movements’ associated masticatory muscle contraction patterns. ICAGD has been repeatedly shown to successfully treat Occluso-muscular pain symptoms without requiring the treated patient to wear a splint or deprogrammer.20–32
This Case Report describes an institutionalized from depression headache patient, that had his prolonged pretreatment Disclusion Times reduced to short Disclusion Time with bonded canine additions followed by the ICAGD coronoplasty. Shortly thereafter, the patient’s pre-treatment chronic headaches were markedly reduced, which led to the patient living with an improved emotional state.
Case Report
A 17-year-old single male, pursuing a Bachelor of Arts was referred from the Neurology clinic with complaints of a 5-year history of chronic right sided headaches. The headaches were acute in onset, intermittent type, prickly in nature, with mild-moderate intensity, radiating from the right side of his face towards his jaw. These headache episodes were often accompanied with nausea and photophobia, along with the patient withdrawing from his surroundings. The headaches were aggravated by stress that coincided with his learning new information related to his academic tract.
The patient’s past history indicated at the age of 10 he became obsessive compulsive, which lasted for 1 year and then spontaneously disappeared. The family had no history of significant illnesses or history of migraine. His headache onset occurred during high school, which the patient finished with average scholastic performance. During his higher studies after high school, the patient experienced further worsening of his headaches, advancing from 1-2 episodes per week to 4-5, always accompanied by debilitating side effects. He developed progressively more frequent catastrophic thoughts, fearing the potential onset of a severe headache. At times, his parents observed him experiencing significant anticipatory anxiety, when he shivered with fear while his heart pounded, being overly preoccupied with thoughts and fears of his next painful headache. Alarmed by the severity of the headaches, and of his fearful behaviour in response to them, his parents consulted various neurologists in search of a causative neurologic disorder, and with a psychiatrist to assist the patient emotionally. The patient’s neuroimaging and Electroencephalography (EEG) were both normal, such that over the next several years, the patient continued to regularly use analgesics, experiencing a partial improvement in symptoms but no remission. His pain gradually worsened in frequency and intensity, but no known precipitating factors were isolated, which led the patient to experience further emotional distress.
When the patient initially presented to outpatient Psychiatry, he reported pain symptoms lasting for 2-3 hours that occurred 3-4 times a day, despite using pain medication. He stated he could feel his heart racing, he would sweat, and sometimes he had difficulty breathing. He described his headaches “as excruciating,” when they pulsated anterior to both ears. The patient also complained of pain in his jaw, fatigue while chewing, and difficulty chewing hard foods. Emotionally at intake, the patient expressed a lack of interest in doing daily activities, he was unable to sleep (insomnia) and had occasional self-death wishes. He felt very low and hopeless about his situation, rationalizing that ‘it would be better to die than to suffer like this.’ In view of these wide-ranging physical and emotional symptoms, the patient was then admitted for observation, evaluation, and management.
The patient’s systemic examination was unremarkable, and an otorhinolaryngologist reported the patient’s ears, nose, and throat were all normal. The patient scored 9-out-of-10 on a Visual Analog Scale (VAS)33 that assessed pain levels and quantified the patient’s severe depression that included him having fleeting death wishes. A clinical diagnosis of moderate depression without somatic symptoms was made, as per the DSM-5 and the International Classification of Diseases 10 (ICD10). The patient’s oral examination revealed there was an anterior open occlusion with very shallow canine guidance contacts bilaterally, and a number of misaligned teeth (Figure 1). As the patient felt noticeable tenderness over his right maxillary area, a dental referral was made to evaluate the patient’s occlusion for potentially contributing to his headache condition.
The patient received a Temporomandibular Joint Vibration Analysis (JVA), a jaw motion analysis using the JT-3D incisor-point tracker, and a muscle analysis using the BioEMG III electromyograph (Bioresearch Associates, Inc. Milwaukee, WI, USA) (Figure 2). JVA revealed a right partial disc displacement that occurred very close to opening, and reduced before the next opening cycle (Piper 3a). The left TM joint demonstrated minor disc movement.
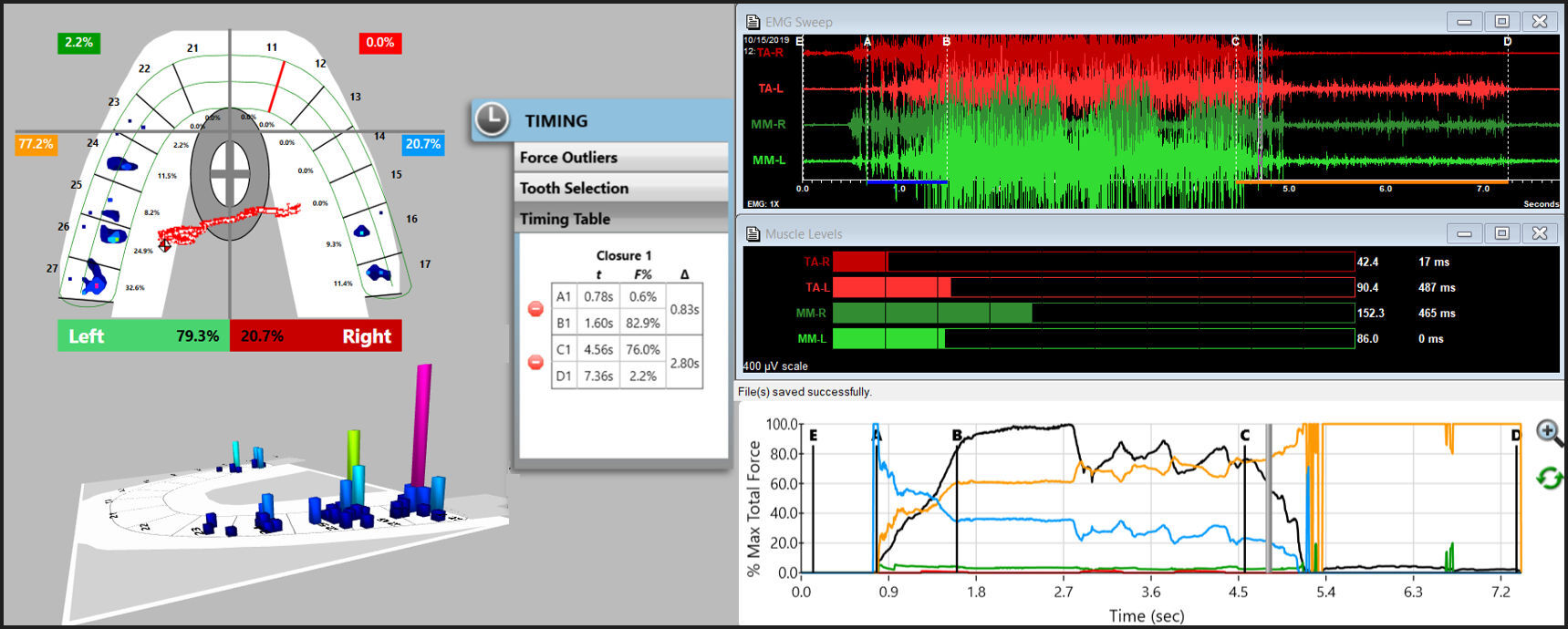
This exam was followed by a T-Scan10/BioEMG III functional analysis of his occlusal force distribution and muscle responses. The patient had four electromyography electrodes placed on his bilateral masseter and temporalis muscles, after which he intercuspated firmly into the T-Scan recording sensor (Evolution HD sensor, Tekscan Inc., S. Boston, MA, USA) to record his closure and excursive movements, and the masticatory muscular contraction patterns related to that occlusal function (Figures 3 & 4).
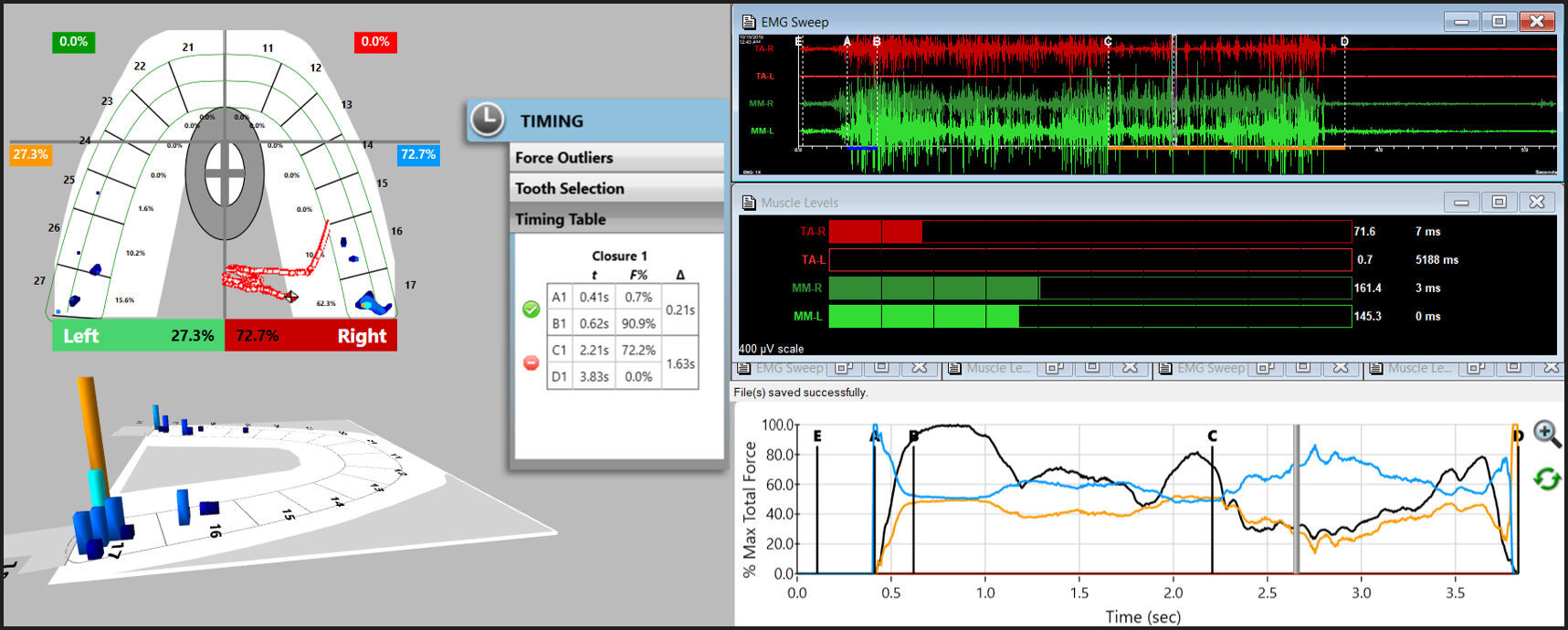
Centric Occlusion was assessed by the patient making a 3-closure Multi-bite recording (Figure 5). This was followed by a left excursive movement recording, where the patient intercuspated firmly into the T-Scan sensor, held his teeth in Maximum Intercuspation (MIP) for 1-3 seconds, and then glided left out to the tips of his opposing canine teeth (Figure 6). The right excursive recording was made in the same fashion (Figure 7).
This functional assessment determined there were no internal derangements of significance, but the patient did present with prolonged left and right excursive Disclusion Times (left =1.63 seconds; right = 2.11 seconds), see Figures 6 & 7, indicating there was excess occlusal surface friction present in each excusive movement. The DT values were outside of the known physiologic ranges (DT ≤ 0.4 secs.)21,24 as was also the Time-to-Muscle Shut Down26 of the contracting muscles, which ranged between 1.50 seconds in right excursion to 2.80 seconds in left excursion, both being far too long for good muscular physiologic health. This prolonged excursive muscle firing was a major contributor to the patient’s muscular symptoms and jaw pain. The patient was diagnosed with Occlusal-muscle Disease (OMD) with hyperactive facial muscles and minimal TM joint damage that resulted from his anterior open occlusion causing severe prolonged occlusal surface excursive friction and bilateral prolonged Disclusion Times. The question remained as to whether his headache symptoms were also resultant from the prolonged muscle firing.
It was explained to the patient that his Disclusion Times were too long, causing the excursive muscle hyperactivity that caused his muscular symptoms. He was further informed that his muscular pains could be minimized or eliminated if he elected to have his Disclusion Times properly reduced.
After obtaining patient consent, canine coupling contacts were created with composite and installed bilaterally (teeth #s 13-43; #s 23-33), to create functional anterior guidance surfaces that would control the patient’s (soon to be) new right and left excursions (Figure 8). The ICAGD coronoplasty was then performed on his right and left excursive movements as previously described,11 to remove the prolonged occlusal surface friction and reduce the DTs to within physiologic limits. Post ICAGD, the multi-bite, left excursive and right excursive movements were recorded in the same fashion as pre-ICAGD (Figures 9, 10 & 11). When the patient closed firmly into his new Maximum Intercuspal Position (MIP), the symmetry, synergy and firing patterns of the bilateral masseter and temporalis muscles were improved from pre to post-ICAGD (Figure 9). The corrected left excursive DT = 0.27 seconds (Figure 10), and the corrected right excursive DT = 0.29 seconds (Figure 11). Compared to the pretreatment excursive EMG hyperactivity (Figures 6 & 7), the post ICAGD excursive muscle activity levels were markedly lessened after the ICAGD treatment (Figures 10 & 11). Additionally, the Time-to-Muscle-Shut-Down of all muscles in both excursions was drastically shortened after ICAGD (right = 0.16 seconds; left = 0.19 seconds).
As was observed in this clinical case, the reason that ICAGD is effective in treating Occluso-muscle Disorder symptoms is that the computer-guided, time-based occlusal adjustments, ultimately shorten the contraction times of the involved muscles that move the mandible excursively. Less contraction time allows for lactic acid clearance that removes the toxic byproducts of tooth-induced muscle contraction. Then the ischemic and painful muscle fibers can re-oxygenate properly, which aids greatly in muscle fiber healing and muscle performance recovery.26
The patient was followed after the ICAGD procedure, when he reported significantly reduced frequency and severity of his headaches. Within a few days’ post DTR/ICAGD treatment, he was discharged from Psychiatric inpatient care, without being prescribed any psychotropic medications. He was advised to reappoint if his headache problem noticeably recurred.
Twelve months’ post-discharge, the patient was followed up over telephone. He had resumed his studies and wanted to focus on his career now that his pain was only occasional, and its’ severity came down appreciably. A 12-month post ICAGD VAS score was obtained that was only 2-out-of-10. In the hopes of obtaining a long-term physiologic result, the patient entered into orthodontic treatment to address both his misaligned teeth and his anterior open occlusion.
Discussion
This clinical outcome aligns very closely with all of the numerous previously published papers describing the rapid physiologic healing effect that Disclusion Time Reduction with ICAGD offers myogenous TMD sufferers that are also emotionally compromised from living in chronic pain.10,16–32 Specifically, this Case Report described a severely depressed patient with suicidal tendencies. His severe mental state was related to that no isolated physical neurologic causes for his headaches were found, and that he failed to gain headache resolution with psychiatric treatment and repetitive pain medication use. However, the biometric diagnostic analyses the patient underwent did isolate a known symptom-causing physiology,16–32 that many studies show cause muscular head, face, and neck symptoms.16–32 As such, the authors elected to treat this patient’s high excursive muscle firing and spasm occlusally with ICAGD. Once the patient’s chronic headache pain was removed from his existence, the fear of headache onset lessened, and his emotional depression also lessened. The absence of the physical elements of this patient’s headache condition (pulsating temporal pain, jaw pain, chewing fatigue, nausea, and inability to sleep), led to the patient experiencing less anticipatory anxiety. The episodes of heart pounding and death wishes were replaced with calmness and an improved life outlook.
Importantly, the dentist is not a psychiatrist and has no way of knowing how the severity of any single patient’s mental state could influence the rendered treatment’s acceptance or lack thereof. Therefore, when severe psychological disturbances are a component of the patient’s clinical presentation, it may be helpful to initially render an alternative to definitive occlusal intervention, such as splint therapy.
This Case Report is another example illustrating that muscular TMD symptoms and headache respond well to occlusal adjustment therapy that is guided by precise closure and excursive timing measurements. This patient’s response mirrors that which has been reported in many published ICAGD studies and clinical reports,16–32 since the inception of the first T-Scan I technology in the mid 1980’s.17,21,34,35 Consequently, treating Occluso-muscle dysfunction with ICAGD is not new. Lengthy Disclusion Time has been shown in EMG studies to elevate excursive muscle activity levels, and that proper reduction of the Disclusion Time to ≤ 0.4 seconds, can reduce the muscle hyperactivity and related Occluso-muscle pain symptoms.16–33
However, this patient’s clinical outcome directly contradicts many articles that had (incorrectly) concluded that chronic pain physical symptoms are secondary to agitated emotional states.4,6,36–39 These studies were all accomplished without measurement of the occlusion or the muscle physiology, without the T-Scan 10/BioEMG III technologies. The absence of any quantifiable occlusal physiology measurements allowed these authors to perpetuate the idea that occlusion does not have a role in chronic pain symptoms. But this Case Report clearly shows the reverse, and instead corroborates both the 83 depressed subject ICAGD/DTR/Beck Depression study results,10 and the many other ICAGD/DTR studies where chronic pain subjects had their physical pains reduced statistically with precision occlusal adjustments.16–32
ICAGD lessens hyperactive muscles from within the Central Nervous System (CNS), by controlling the molar Periodontal Ligament (PDL) mechanoreceptors and pulpal nerve fibers, which synapse directly with efferent motor fibers that contract the four masticatory muscles, along with the Swallow Mechanism muscles.40 Prolonged excursive frictional contacts increase the total time the pulp is flexed and the PDL mechanoreceptors are compressed during excursive movements. Both the pulpal flexure time and the PDL compression time is equal to the Disclusion Time duration of that same excursion.19 The more the time of the excursive interference contacts, the longer the time of the periodontal fibers are compressed and the pulpal fibers are flexed, resulting in prolonged durations of masticatory muscle contractions.19,21,24 By reducing the length of time the posterior occlusal surfaces contact excursively, the volume and duration of the pulpal flexure and PDL mechanoreceptor compressions are reduced, thereby interrupting the muscle hypercontraction. Post ICAGD, the pulp and PDL no longer hyper-stimulate the involved muscles into a painful ischemic state, allowing for re-oxygenation and muscle fiber recovery that leads to symptom resolution. Importantly, many studies repeatedly show that properly performed ICAGD is a marked improvement in the treatment of muscular TMD symptoms in patients who present with minimal TM joint structural breakdown, compared to the more common unmeasured Occlusal Equilibration involving manipulation into Centric Relation manipulation.14,41 ICAGD is an alternative to splint therapy, to taking analgesics, muscle relaxants, or anti-inflammatory medications, and to trigger point and/or Botox injections.
In this patient’s case, he used analgesics for many years that were unable to bring about any true resolution. Like the many differing symptomatic therapies, medications do not alter the causative neurologic pathway that emanates from the pulpal and PDL fibers, that fire when posterior teeth repetitively compress and flex during occlusal contact. That neural output can only be physically muted neurologically, by controlling the time-durations posterior teeth frictionally engage.
Acknowledgement
The authors thank Prof. Dr. Nagesh K. S. for all his advice.
Funding Statement
No funding was received from any institution or funding agency for the production of this Case Report study.
Conflict of Interest
The 2nd author is a Consultant for Tekscan Inc., S. Boston, MA, USA, and receives no compensation for sales of any Tekscan products.
Author Statements
Prof. Prafulla Thumati: Drafting/revision of the manuscript for content, including medical writing for content; Major role in the acquisition of data; Article concept or design; Analysis or interpretation of data
Dr. Robert B Kerstein: Drafting/revision of the manuscript for content, including medical writing for content; Article
concept or design; Analysis or interpretation of data
Dr. Naveen Manohar Pai: Psychiatric treating practitioner contributing patient care information who participated in the psychiatric diagnosis
Dr. Niharika Singh: Psychiatric treating practitioner contributing patient care information who participated in the psychiatric diagnosis
Dr. Sundarnag Ganjekar: Psychiatric treating practitioner contributing patient care information who participated in the psychiatric diagnosis
Dr. Santosh K. Chaturvedi: Psychiatric treating practitioner contributing patient care information who participated in the psychiatric diagnosis.

_along_with_the_electromyograph_(emg)_were_set_in_place_on_the.jpeg)








_along_with_the_electromyograph_(emg)_were_set_in_place_on_the.jpeg)