INTRODUCTION
Much has been published on Meniere’s Disease (MD) which was first identified and characterized by Prosper Ménière over 150 years ago.1 Today diagnosing and treating MD among clinicians remains challenging2–7 and as a result MD continues to be a catchall for vertigo of unknown origin. Endolymph Hydrops (EH) remains a histologic finding in most but not all MD cases, while the MD diagnosis remains purely a clinical diagnosis. There is no agreement on the etiology of MD as it relates to endolymphatic hydrops.8–15 Current considerations is that EH is a histological sign of the disease rather than a causative etiology.5,9–15 Some research has attempted to induce MD by increasing the endolymph production or limiting its reabsorption through medications. Those models did produce EH but did not produce MD symptoms.16–18 Even if EH does have some influence over vertigo, it does not adequately explain the persistence of tinnitus, ear fullness, or hearing loss progression.
In an attempt to bring clarity to the Ear, Nose and Throat Physicians (ENT) community a few consensus statements and reviews have been published.7–13 The American Academy of Otolaryngology – Head and Neck Surgery published a clinical practice guideline on MD6 with the stated purpose: “To maximize treatment, it is important to clinically distinguish MD from other independent causes of vertigo that may mimic MD and present with hearing loss, tinnitus and aural fullness.”6 Even though TMD is known to present with this same presentation of symptoms,19–31 the AAO-HNS fails to make any mention of the similarities in inner ear symptom presentation between TMD and MD anywhere in its 55-page guideline. This is counter intuitive if the aim of their guideline is to distinguish MD from other causes that could mimic MD symptomology. It is well known that James Costen, an otolaryngologist, first read his initial findings of inner ear and sinus symptoms related to disturbed function of the TMJs in 1933 before the Texas Ophthalmological and Otolaryngological Society and was later pubished.32 Subsequently he followed 125 cases through prosthetic treatment and published his findings in 1936.33 Most of the 125 patients were partially or fully edentulous creating a loss of molar support, but a few had a full complement of perfectly normal teeth. All were referred to a dentist for various needed prosthetic treatments. For those with normal teeth a 2 mm to 4 mm overlay successfully relieved their symptoms.33 This was the first report of the use of an oral appliance to relieve TMD that has become so prevalent today. Costen hypothesized that the loss of molar/premolar support resulted in overclosure, distalizing the condyle, increasing pressure on the eustachian tube, the auriculotemporal nerve, irritating the sensory nerves in the capsule, inducing reflex neuralgia of the proximate branches of trigeminal nerve, irritation of the chorda tympani and that these were multiple etiologic factors of the oral, facial and ear pains, catarrhal deafness, tinnitus, and vertigo associated with MD.34 However, he concluded that malocclusion could also result in MD symptomology and that TMJ X-rays could contribute to a more accurate diagnosis of many MD cases.
More recent authors have subsequently labeled his work Costen’s Syndrome, which eventually became known as TMJ Syndrome and currently is labeled as Temporomandibular Disorders (TMD). In the early 2000’s research spearheaded by Bjorne et al began establishing a link between TMD and MD.30,35–37 Treating TMD patients that were also diagnosed with MD resulted in complete resolution of the MD (and TMD) symptoms or decreased to a level they no longer were life altering for the patient. The symptom resolution was long term as indicated by 3-year and 6-year follow up studies.35,36 Treatments rendered were occlusal adjustments, TMD splint therapy, cervical spine therapy and physical therapy.36–38 It was impossible to know if one therapy was responsible for the therapeutic outcome, or if there was a result of a synergistic effect of all the employed therapies. A few case studies have shown occlusal adjustments to be highly effective in treating patients that have been diagnosed with Meniere’s Disease.38,39 This study will only use bite revision therapy via DTR in an attempt to bring symptom relief in a cohort of 86 subjects with a diagnosis of MD. DTR has demonstrated effective and long-term symptom resolution in known TMD and Orofacial pain patients.40–49
What is Joint Vibration Analysis (JVA)?
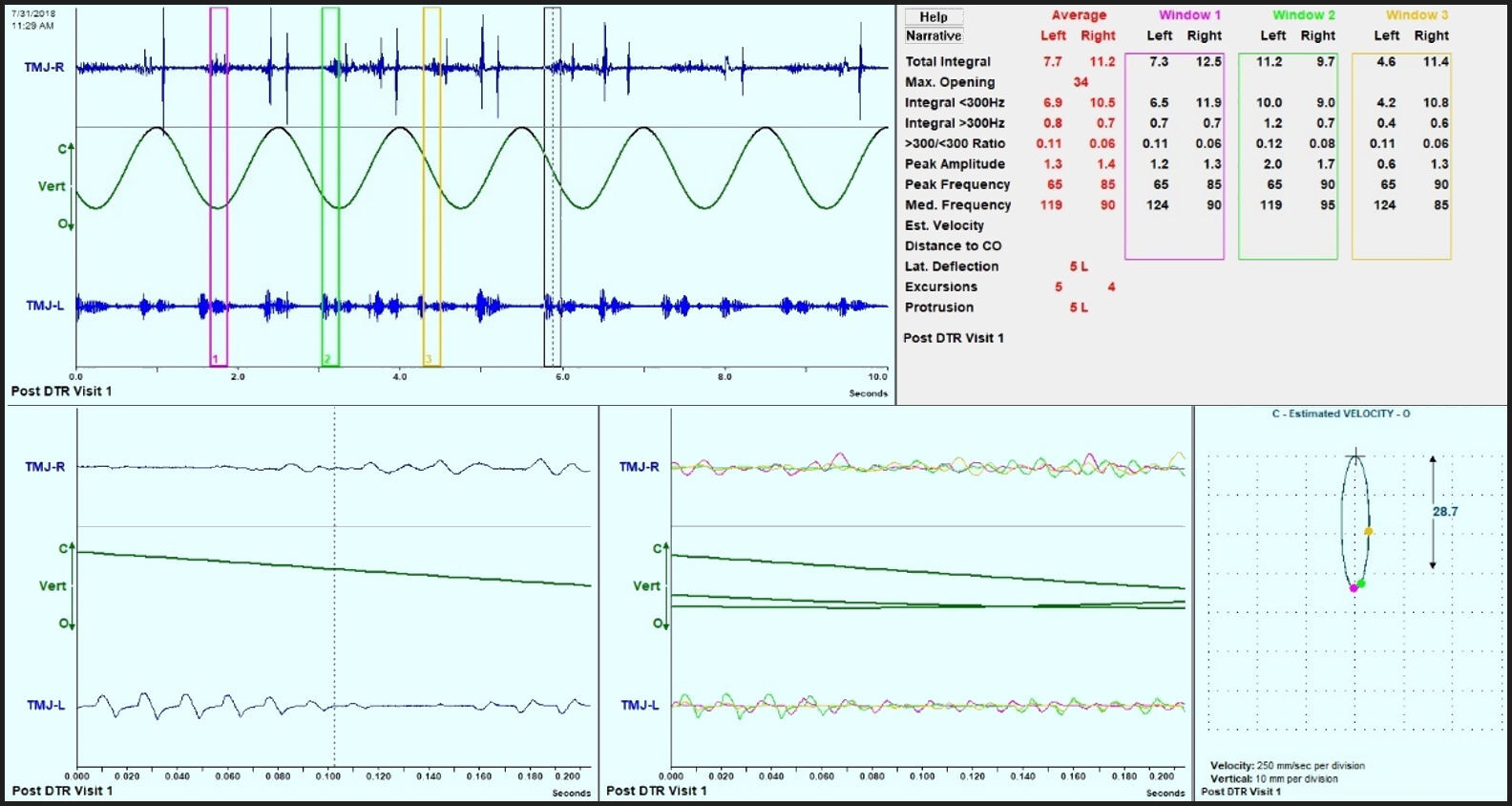
JVA of the temporomandibular joint (TMJ) is the process of using accelerometers that are positioned over the TMJs (see Figure 1.) to record vibrations that occur inside the joints during movement, 2) to evaluate the intensity and frequency content of the vibrations and then 3) comparing those values to known values from previous verified examples. The subject opens and closes throughout the full range of motion from maximum intercuspation repeatedly for a minimum of 6-8 cycles and taps their teeth together at full closure. This allows the operator to classify any vibration into categories like late opening or early closing vibration for example. The recording is displayed as a sweep graphic showing mandibular motion and right and left vibrations for several cycles. The authors used JVA to quantitate the vibration in the joints before and 6 months post therapy. See Figures 2 and 3 respectively for examples. It has already been established that occlusal corrections can improve range of motion and joint vibrations.50
OBJECTIVES
The objective of this cohort study was to perform DTR Therapy on patients with a confirmed diagnosis of MD who presented with long Disclusion Times and/or a bite force imbalance, with high excursive muscle activity levels, all of which could promote MD and joint symptoms. The results of this pilot study will either corroborate or contradict the prior case report’s that observed MD symptom reductions that followed the measured occlusal adjustment therapy.38,39
METHODS
Eighty-six patients previously diagnosed by an otolaryngologist (ENT) physician with Meniere’s Disease (MD), were evaluated in two different dental practices that offer specialized Disclusion Time Reduction TMD services. All patients had prior magnetic resonance imaging (MRI), which ruled out auditory neuromas. All the patient’s had tried various treatments from dietary restrictions such as avoidance of salt and caffeine to inner ear gentamycin and stem cell injections. None of these treatment options brought about relief for any length of time. The sampling method used in this study is a “convenience sampling.” One general dentistry office located in Eugene, OR where 32 consecutive patients diagnosed with MD were seen that met the inclusion criteria were evaluated and treated. The second dental office located in RajaRajeshwari Dental College, Dept of Orofacial Pain under Rajiv Gandhi University of Health Sciences in Bengaluru India. The Department of Ear Nose and Throat at RajaRajeshwari Medical College was contacted to seek out patients that met the inclusion criteria sent to the second dental office to be evaluated and treated. An IRB exemption was requested and obtained for a retrospective cohort study #BIRB/99Z/2022.
The Inclusion criteria were:
-
A MD diagnosis from an otolaryngologist with MRI that definitively ruled out an auditory neuroma
-
The existence of ongoing MD symptomatic episodes
-
28 teeth with symmetrically missing teeth (if one molar was missing on the left side, then one had to be missing on the right side)
-
Near normal occlusal relations with molars and premolars in contact during the right and left excursions
-
Angles Class I and Class III occlusal relations, with guiding anterior teeth that were either in contact, or near to contact
-
Patients that had been previously treated for MD but did not receive symptom resolution
-
Patients 18 years of age or older
The Exclusion criteria were:
-
Severe Class II malocclusions and anterior open bite where anterior guidance contact could not be achieved
-
A previous history of TMJ trauma
-
The presence of unstable Temporomandibular Joint internal derangements verified by CBCT and/or Joint Vibration Analysis (JVA).
-
Patients that had been previously treated with MD therapy that received symptom resolution
-
Patients who had undergone prior TMD therapy, including prior occlusal adjustment treatment.
-
Patients younger than 18 years of age
DESCRIPTION OF THE DTR THERAPY
The therapy is described elsewhere in detail.40,51 Briefly, teeth were dried on one side of the mouth (top and bottom), then the subjects closed into their Maximum Intercuspal Position (MIP) with 21-micron thick articulating paper (Parkell, Englewood, NY, USA) between the teeth. Then the subject moves into a right excursive all the way out to the tip of the canine, then back into MIP, then this excursive
movement is repeated to the left and back into MIP. The pre-treatment recordings then guided the authors to the appropriate areas of occlusal surfaces that necessitate corrective adjustments. The posterior working and non-working lateral interferences are completely removed and centric stop contacts are revised from broad contacts into small pinpoint contacts located on supporting cusps, marginal ridges and central fossae. This is then repeated on the opposite side.
DTR therapy was considered complete when
-
All lateral posterior excursive interferences are removed
-
Disclusion times had measurably been reduced to <0.5 seconds in both directions
-
Habitual closure contacts were located solely on cusp tips, fossae and on marginal ridges
-
T-Scan revealed that patient self-closure into MIP achieved bilateral simultaneous force rise
Post therapy recordings were taken in the same fashion as the pre therapy recordings to confirm disclusion times were correct. Patients were seen at day 1, at one month and 3 months to refine the above procedure. This allowed muscles and TMJs to heal after the occlusal corrections. JVA recordings were taken pre DTR and 6 months post DTR completion and JVA data compiled.
Joint Vibration Analysis Parameters Defined52
Total Integral - The area under each vibration’s Fast Fourier Transformation (FFT) frequency distribution curve in units of KiloPascal-Seconds. It is the best measure of the overall intensity of a vibration by combining all frequencies present. See Figure 4.
Integral < 300Hz - The area under the vibration FFT distribution curve from 30 Hz to 300 Hz. These frequencies are associated with soft tissue-initiated vibrations such as disc displacements and reductions. See Figure 4.
Integral > 300 Hz - The area under the vibration FFT distribution curve above 300 Hz. These frequencies are associated with hard tissue-initiated vibrations such as degenerative joint disease. See Figure 4.
Peak Amplitude - The most intense frequency within the entire FFT frequency distribution. See Figure 4.
Peak Frequency - The single frequency at the peak amplitude level. See Figure 4.
The Wilcoxon Signed-Rank test was chosen for analysis between the pre-treatment means and the post-treatment means of this group due to the recognition that some of the data did not occur normally distributed according to the Shapiro-Wilk test.
RESULTS
The objective of significantly reducing mean disclusion times was accomplished in this study. See Table 1.
Significant reductions in the left TMJ vibrations post-DTR included the means of; a) the Total Integral (p < 0.0002), b) the < 300 Hz Integral (p < 0.00012), c) the > 300 Hz integral (p < 0.01876), d) the Peak Amplitude (p < 0.00005). The Ratio (> 300/< 300) exhibited a trend towards a reduction (p = 0.07078), while the mean Range of Motion increased significantly (p < 0.00001). The mean coefficient of variation of the left parameters was significantly reduced post DTR (p < 0.0127). See Table 2.
Significant reductions in the right TMJ vibrations post-DTR included the means of; a) the Total Integral (p < 0.00047), b) the < 300 Hz Integral (p < 0.00001), c) the > 300 Hz Integral (p < 0.00193), and the Ratio (p < 0.00034). A significant reduction in lateral deflection at maximum opening was also revealed post treatment (p < 0.01618). The mean coefficient of variation for the right parameters was also significantly reduced (p < 0.0127). See Table 3.
DISCUSSION
The null hypothesis was rejected.
It was observed that the mean patient range of motion increased significantly, suggesting that some of the TMJs were operating with less restriction or muscle relaxation was greater post DTR.53 Meanwhile, both the left and the right TMJ vibrations were significantly reduced according to the parameters (< 300 Hz, > 300 Hz) by about 50 %. Less vibration equals smoother function, which is typical of asymptomatic subjects with good masticatory function.42,50
It is interesting that MD patients are responding to DTR therapy in the same manner TMD patients do. The observations that known MD symptomology improved or resolved with mastication improvement concurrently while TMJ improvements were noticed, leave little doubt that MD is not its own disease process.
It is known that secondary otalgia accounts for 50% of all types of inner ear pain, and 50% of that secondary otalgia is of dental origin.54 Yanagisawa & Kveton studied 615 patients and concluded the most common causes of secondary otalgia were dental (38%), and 35% of Temporomandibular Joint Disorders (TMJD) proposing that up to 73% of secondary otalgia had a dental origin.55
The authors propose the direct therapeutic mechanism(s) for the observations made during the treatment of these subjects.
Neurologic Component
It is common knowledge that the motor division of the trigeminal nerve innervates the masseters, temporalis, lateral pterygoid, medial pterygoid and tensor tympani. In part 1 we observed hyperactive muscles relax to a “normal” or lessened activity state by controlling PDL compression input to the trigeminal motor nucleus. The tensor tympani is responsible for impedance of sound in response to auditory and non-auditory stimuli.3 Whatever the reason, contraction of the tensor tympani results in low frequency-mixed hearing loss.56 It is likely that the tensor tympani would also behave in the same manner of relaxation as there is a neurologic pathway described in Haines.57 Afferent mechanoreceptors from the molar and premolar PDLs enter the Central Nervous System (CNS) in the Mesencephalic Nucleus, and travel onwards to the Trigeminal Nucleus,57 where they synapse directly with efferent motor fibers to the muscles innervated by the CNS. Also innervated by these motor efferent fibers are the mylohyoid, the anterior digastric, the tensor veli palatini, and the tensor tympani muscles.57 This direct neural connection between the posterior teeth PDLs and the tensor tympani muscle, is likely one component contributing to the symptoms of MD. Vass et al reported that there exists direct trigeminal innervation of the inner ear vasculature which provides for rapid and possible sustained vasodilation responses of the inner ear to excitatory levels of activity and sensory input. This provides an alternative and contributory mechanism for observed clinical disturbances including imbalance, hearing loss and tinnitus.58
Musculoskeletal Component
Abnormal muscle contraction affecting disease states has been recognized and has a long-standing history in Medicine. In 1876 Lewis Sayre, MD, an orthopedic surgeon, noted that rotary lateral curvature of the spine had nothing to do with a disease state of the bone, but rather the observed “distortion was dependent entirely upon irregular muscle contraction.”59 Professor Sayer also described a case where a knee was disarticulated and luxated backwards, as a consequence of chronic inflammation due to irregular muscle contraction.60 He stated that muscle will deform limbs and bones, according to the strength and power of the muscles involved in the contraction and will guide the deformity of the bone.60 In growing a healthy skeleton, bone adapts to biomechanical changes in stature, mass, proportionality, body shape, and body composition. Mechanical strains or applied forces are required to deform or change bone, and these forces are predominantly generated by muscle contraction.61 More recently, a study of mammalian mastication suggested that a previous model that described a fully ossified skull as having interlocking bones that formed a single structure, is probably incorrect.62,63 Further, cranial bone mobility has been observed and measured in adult humans, both radiographically and via ultrasound.64,65 By employing surface EMG, the authors recorded abnormal muscular hypercontraction in both temporalis muscles before therapy (See Figures 2-5 in Part 1),66 which after therapy, became a more relaxed temporalis contraction signature. The temporalis is unique, in that its’ attachments encompass five bones67 coronoid process of the mandible, the frontal bone, the greater wing of the sphenoid, the parietal bone and the temporal bone. Knowing that muscles can deform bone, and that both temporalis muscles were hyperactive in this patient prior to DTR therapy, one could postulate that the patient’s sensitivity to sound and/or any hearing loss, may have been partially attributed to a tightening/alteration of the tympanic membrane resulting from temporal bone deformation from the observed temporalis hyperactivity. It is also possible this same bone deformation from the same muscular hypercontraction could compress or otherwise alter the shape of the vestibulocochlear organ, as it is completely encased within the temporal bone, thereby inducing vertigo with no change in fluid amount or composition. Even the slightest bony shape alteration could change the shape and ultimately, the function of any organ inside the bone being altered. These subjects had long Disclusion Times that accompanied their MD condition. After DTR corrections, the volume of their PDL compressions were markedly lessened, because the friction between opposing occlusal surfaces had been adjusted out of their excursive function. This allowed the MD patient’s muscles to relax from a hyperactive state into a more physiologic state, thus returning any aberrantly manipulated bones to a physiologic level of bone tension. After DTR, the symptoms of MD rapidly abated, similar to how many TMD symptoms often resolve after DTR therapy. Both MD and TMD symptoms have been known to wax and wane with time, and it is possible this patient went into spontaneous remission at the initiation of the occlusal therapy. However, the current model of MD does not explain the patient reported improvements in hearing, aural fullness, sensitivity to sound, vertigo, and the lessening and eventual cessation of the medications used to control symptoms, all of which followed the computer-guided occlusal therapy employed with this MD patient. There are only four possible explanations for the observations made in the treatment of this MD patient:
The subjects had two different active disease states occurring concurrently, that resolved at the same time following DTR therapy
This is possible for one or a few subjects across a long period of time. It is not probable that all 86 random consecutive subjects expressed two disease states simultaneously.
There exists a different type of MD that involves dental occlusion
This is possible, but not probable. If different types of MD existed, the results would have had a bimodal distribution presentation. In other words, subjects with only inner ear type MD would not have responded to DTR therapy while subjects with occlusal type MD would have. This outcome was not observed.
MD is one of the many conditions labeled as TMDs
This is entirely possible. Currently, TMD is held as an umbrella term which encompasses at least 40 separate diagnoses. It would be challenging to winnow out MD as a subset on its own. Regardless, these subjects responded to a known TMD therapy with the same results as TMD patients do. If TMD and MD are subsets of one another, how can a proper diagnosis be rendered in an absence of dental occlusal data?
MD was a misdiagnosis, and the subjects instead suffered from TMD
This is the most likely scenario. All the MD diagnosed subjects reported more symptoms than the hallmark MD symptomology, and responded to a known TMD therapy in the same manner that TMD subjects have in past research studies.68–70
Regardless of the suggested explanation of what occurred, these authors caution it would be prudent for the AAO-HNS to recommend that medical doctors rule out TMD as a possible contributory component of the MD symptoms if not the actual etiology. In this MD study of 86 subjects, dental etiology was overlooked, possibly because of limited diagnostic data that lacked occlusal function measurements, specifically the data that is needed to establish the TMD diagnosis. Given the current body of literature on MD, this proposed mechanism must be considered a viable possibility, because over the past 150 years, the medical profession has failed to prove that an abnormal amount of, or composition of inner ear fluid, is the etiological cause of MD. It is important to mention that even considering the absence of a control group, all patients have a history of previously failed MD conventional treatments. Also most of the subjects had suffered for years before ending up in this study, indicating that without the intervention, it is most likely that the condition would have followed its natural course.71,72
CONCLUSION
Eighty-six subjects with confirmed diagnoses of Meniere’s Disease experienced reductions in frequency, duration and intensity of their MD symptoms following reductions in Disclusion Time and muscle activity via DTR through computer guided coronoplasty. Pre and post DTR JVA recordings elucidate that there exists a TMD issue in this patient group diagnosed with MD that had significant improvement post therapy. Although occlusion has been overlooked in most of the medical and dental literature as a possible etiology of MD, the results of this study point to malocclusion, specifically bite force and bite timing, as the etiology for the symptoms in this group of subjects diagnosed with MD. Any provider considering MD as a working differential diagnosis should eliminate TMD as a possible (probable) diagnosis before accepting a diagnosis of Meniere’s Disease.
“It is a central truth of science and medicine that ideas that precede the technology to prove or disprove them, lie fallow” - Janetta
DISCLOSURE
Ben A, Sutter - operates a private practice in Eugene, OR USA, is an adjunct Professor UNLV School of Dental Medicine Department of Clinical Sciences and a member of the Vivos Faculty. USA.
Prafulla Thumati is professor of prosthodontics at Rajarajeswari Dental College and Hospital, Bengaluru, India.
Roshan P. Thumati practices Orthodontics and Dentofacial Orthopedics, COPE Dental Health Care Center, Banashankari, Bengaluru, India.
John Radke is Chairman of the Board, BioResearch Associates, Inc. Milwaukee, WI USA.
FUNDING STATEMENT
No funding from any source was provided to complete this study.