Section I. Background
The widely advocated, but unsupported philosophy that “occlusion plays no role in the etiology of chronic Temporomandibular Disorders (TMDs)” has been extensively taught worldwide in dentistry. Some professors, especially dental researchers not involved in treating TMDs patients, have taught that negative emotions are etiologic of chronic pain and other TMDs symptoms.1 These teachings have also negatively biased the dental profession against the TMDs patient diagnostic and treatment benefits that biometric (electronic and computer-enhanced) technologies bring to improve the accuracy of diagnosis and treatment of TMDs.1 And although it has been repeatedly confirmed that painful TMDs can incite emotional responses, those dismissing any occlusal etiology have been unable to provide even marginal evidence that TMDs can be effectively relieved with any version of psychological counseling, Cognitive Behavioral Therapy (CBT), or any psychiatric treatment.2–10 This is not a claim against any treatment for mental illness, but it is a claim that TMDs are very rarely mental illnesses.
Some authors have claimed that painful, chronic physical and dysfunctional TMDs symptoms arise from both physiological etiologies, and the emotional anxiety and depression precipitated by a patient’s life stresses.6,7 The Myofascial Pain Dysfunction Syndrome (MPDS) theory from 1969 suggested that emotional stress and anxiety exacerbated physical stressors upon the Stomatognathic System, which caused the development of chronic painful symptoms. However, only vague and unrepeated evidence has been forthcoming since the 1980s to support that theory.2–7 Others have hypothesized that myalgia may be Central Nervous System (CNS) mediated, but to date there is minimal scientific evidence to support that hypothesis. Regardless of the potential etiology, it is widely accepted that living with chronic masticatory muscle pain is frequently associated with negative emotional sequelae.11,12 Strong scientific evidence supporting occlusal involvement comes from computer-guided occlusal adjustment studies that resolved painful TMDs symptoms and demonstrated that direct physical correction of the occlusion also returned TMDs subjects’ emotional states back to normal.11,12
The basic premise of the psychosocial/emotional TMDs etiology theory is that physical muscular pathologies and TMJ structure breakdown occur secondary to anxiety, depression, and/or somatization (SSD), by stimulating clenching and grinding habits that can damage teeth, muscles, and the Temporomandibular Joints.2,7 Another scientifically unsupported contention is that “pain” is the instigator of TMDs, which has focused educators to suggest “pain” is the only relevant TMDs symptom, discounting the importance of physical structural factors as all being secondary to pain. This pain focus has produced only failed studies where pharmacologic agents did not resolve TMDs.8,9 Despite that for the past 30+ years Cognitive Behavioral Therapy (CBT) has been promoted as a valid TMDs treatment, a 2022 systematic review of psychological TMDs treatments found insufficient evidence that psychological therapies resolve painful TMDs.10
If TMDs were likely to be caused simply by stress and anxiety, alleviating those stressors should result in the remission of all symptoms, at least in the relatively acute cases. Further, if emotional stress does result in physical trauma, relieving the emotional stress should allow healing of the physical structural damage. However, that has never been demonstrated in any scientific study.6,10 If a strict emotional etiology of TMDs were true, occlusal change should have no positive effects. But physical treatment has been shown to relieve physical damage, its associated pain, and simultaneously resolving the emotional factors, despite multiple etiologies.11,12
Studies have supported that TMDs painful physical symptoms can be reduced or eliminated by removing specific functional occlusal interferences with the well-established Disclusion Time Reduction (DTR) coronoplasty procedure. Concurrently, depression, anxiety, incorrectly perceived somatic symptoms, and patient overall psychological well-being have been improved according to validated psychometric instruments.11–14 Furthermore, the resolution of Meniere’s Disease and Trigeminal Neuralgia (both accepted TMDs) have been successfully treated with DTR occlusal therapy in lieu of cognitive behavioral therapy or other counselling.15–19
Five Explanations that Refute Discounting Occlusion as a Potential Cause of TMDs
There are five scientific explanations that refute the unsupported claim that “Occlusion Plays No Role in TMDs:”
-
The claim completely ignores both the complex neuroanatomy that dental occlusion has because of its afferent connections into and within the Central Nervous System (CNS), and the extensive efferent connections from deep within the CNS to physically cause chronic TMDs symptoms.20,21
-
The proponents of this claim have managed to ignore the vast literature supporting occlusal interferences as a physical causation of TMDs that was first isolated from within the dental occlusion by the T-Scan I technology (Tekscan, Inc. S. Boston, MA USA),22–24 and was subsequently physiologically verified in studies using the T-Scan 7-10/BioEMG III synchronized technologies (Tekscan, Inc., Norwood, MA, USA; Bioresearch Associates, Inc., Milwaukee, WI, USA).25–37 Importantly, over the past 3 ½ decades, T-Scan guided occlusal treatments have repeatedly alleviated TMDs symptoms in many TMDs treatment studies performed by different researchers on different patient populations in different countries.22–37
-
The claim completely ignores the indisputable fact that the world’s two most popular and successful long-term TMDs treatments utilized by clinicians are OCCLUSAL:
-
The placement of a maxillo-mandibular appliance provides an occlusal interface optimized by the clinician, which effectively mutes the complex dental occlusion’s afferent input into the CNS.38
-
Disclusion Time Reduction (DTR) with the Immediate Complete Anterior Guidance Development coronoplasty (ICAGD) selectively treats the dental occlusion’s neurophysiology, utilizing high-precision, time-based occlusal adjustments that remove only real interfering contacts.22–37
If occlusion has no relationship to TMDs, oral appliances and DTR therapy must be viewed as the two most amazingly effective placebo treatments ever devised for the treatment of TMDs.
-
-
The denial of occlusion’s etiologic role is based in part upon the unproven theory that “Central Sensitization” is etiologic for TMDs.39 This minimally supported theory suggests that TMDs symptoms clinically appear when the Central Nervous System (CNS) unexplainedly becomes overly sensitive to external stimuli, which either:
-
Reduces the patient’s pain threshold to mildly painful conditions, thereby heightening the patient’s pain perception of the condition, or
-
Increases the patient’s CNS pain response to their otherwise minimally painful structure(s), such that the structure(s) becomes perceived by the patient as being very painful.
Central Sensitization theory evolved from the equivocal (similarly ineffective) treatment results observed between TMDs patients and control subjects in unmeasured, subjectively performed mock equilibration studies that were published from the 1960s to the 1990s. Neither TMDs patients nor control subjects positively responded to the performed, but unmeasured occlusal adjustments (see Section II). This led the authors of that time to incorrectly assume that occlusion was not a major component of TMDs.7,40–45 Central Sensitization has also been widely postulated to promote Chronic Fatigue Syndrome (CFS), Irritable Bowel Syndrome (IBS), Temporomandibular Joint Disorders (TMJDs), and has been considered comorbid with Fibromyalgia and chronic Vulvodynia Syndrome, which are all syndromes with unknown or poorly understood etiologies. No published scientific study has been able to describe the precise mechanism of CS or substantiate that Central Sensitization exists.
- Importantly, CS theory does not explain how the very selective removal of a few interfering occlusal contacts can completely relieve TMDs symptoms after a diagnosis of Central Sensitization has been previously established.
-
-
The claim that 'Occlusion Plays no Role in TMDs" ignores the fact that research-tested psychotherapeutic and pharmaceutical treatment approaches have both repeatedly failed to resolve TMDs symptoms in ardent published studies,2–10 but TMDs patients routinely respond positively to occlusal treatments.11–19,22–37
SECTION II. How Did “Occlusion Has No Role in TMDs Causation” Evolve?
This incorrect claim harkens back to mock occlusal equilibration studies performed before the T-Scan I technology was developed, along with a few occlusal adjustment studies performed after T-Scan was developed, but without its use.7,40–45 With purposeful biases, the promoters of the “Occlusion Plays no Role in TMDs” theory have managed to ignore twenty-five T-Scan studies since 1991 in which T-Scan timing and force metrics were successfully used to guide occlusal adjustments that completely resolved many TMDs.11–19,22–37
Mock Equilibration Studies
In occlusal adjustment studies that included placebo groups who underwent “mock equilibration” (polishing), treated TMDs subjects received real adjustments based upon the incorrect theory that articulating paper mark sizes indicated force levels.46–48 This contact selection method was widely advocated to be true despite never being scientifically tested until 2007, when it was completely invalidated.49,50 See Figures 1 and 2.
The theory that articulating paper mark size indicated the amount of occlusal force advocated that:
-
Large Dark Marks were believed to represent High Force occlusal contacts
-
Small Light Marks were believed to represent Low Force occlusal contacts
-
Widespread Paper Mark Distribution was believed to represent Simultaneous Timing of all occlusal contacts
Using the articulating paper marks indicate forces theory to adjust the occlusion was incapable of identifying the occlusal contacts that were etiologic of TMDs. A 2007 study totally disproved this paper mark size/force belief system when out of 600 differing sized paper marks, large dark marks were forceful only 14% of the time and small light marks were low force only 14% of the time.49 This meant the authors performing occlusal adjustment studies using paper mark size to choose contacts for treatment would adjust incorrect contacts 86% of the time. This explains why these authors reported no real TMDs improvements in their occlusal adjustment research.7,40–45
An example of this mock equilibration research involved 51 patients that were randomly divided into two groups; 28 subjects received real occlusal adjustments and 23 received mock equilibration. The authors reported the same minimal degree of symptom improvement in both the groups.43 This study and a follow-up paper by the same authors provided good evidence that the subjectively performed occlusal adjustments were no better in treating TMDs than was mock equilibration.44 Rather than interpreting this result as "mock equilibration was as good as real equilibration," the authors could have just as reasonably concluded that the paper mark size equilibration method was no better than mock equilibration. In other words, their real equilibration method was ineffective.
One mock equilibration study in support of the MPDS theory reported that out of 25 subjects who received mock equilibration, 16 subjects experienced “total or nearly total symptom remissions.”41 During the past 50 years this is the only report of successful TMDs treatment using mock equilibration or any other placebo. And although Goodman, Greene, and Laskin’s 50 year-old mock equilibration study has been highly promoted and often referenced, if mock equilibration could reliably induce significant reductions of MPDS symptoms in 2 out of every 3 subjects (as was claimed by the authors),41 it should be one of today’s favored TMDs treatments (minimally invasive, reversible, low cost, painless, easy to provide, a quick source of easy revenue, no training required). Despite all those perceived procedural positives, mock equilibration has not been widely embraced as a popular TMDs treatment, nor has it ever even been considered as a viable TMDs treatment option.
If mock equilibration was “truly effective,” it might have quickly replaced the occlusal splint and/or DTR therapy as the 2 most used treatments for today’s TMDs. However, only one study exists where the placebo effect was reported to control the majority of chronic TMDs symptoms.41 A 67% effective placebo treatment result appears to be too good an outcome, suggesting something may have been wrong with how that study was performed.41
-
The fact is that mock equilibration does not in any way correct the occlusal neurophysiology responsible for TMDs described in Section III.
-
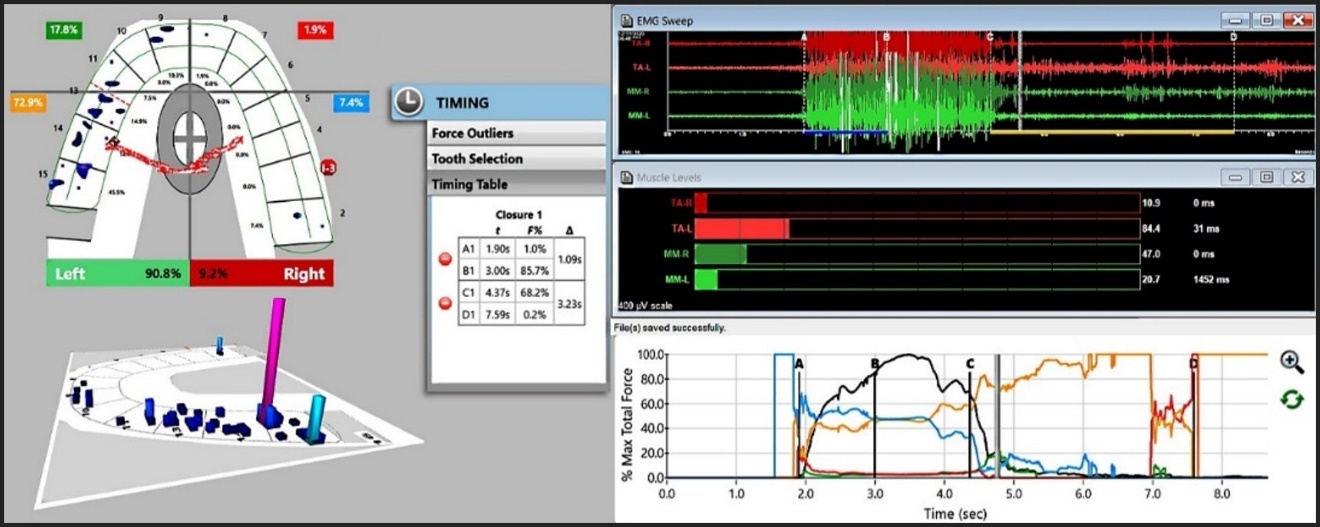
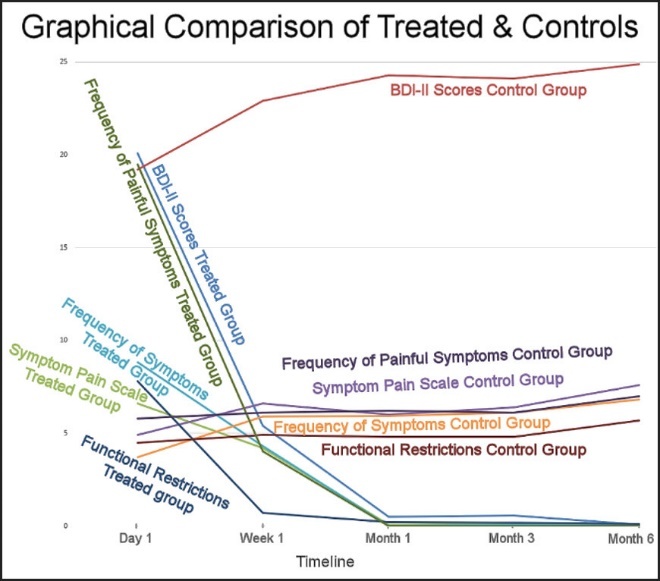
Quite to the contrary, two separate Disclusion Time Reduction Randomized Controlled Trials (RCT) showed TMDs were repeatedly alleviated in the treated subjects while the controls who received mock equilibration got worse over the studies’ durations.14,33 See Figure 3.
Methodological Failures of the Mock and Real Occlusal Adjustment Studies Prior to T-Scan
In all prior mock/real equilibration studies, the adjustments performed (as reported by all authors) were to equalize Centric Relation and Centric Occlusion (CR-CO), and adjust only balancing side contacts.7,40–45 It had long been incorrectly advocated that balancing side contacts caused TMDs, and the CR-CO discrepancy was a focal point to commence bruxing behavior.46–48 Yet in the treated subjects, adjusting CR-CO and balancing inclines did not result in significant improvements of subjects’ TMDs.40–45 It was later understood using the T-Scan 7/BioEMG III synchronized technologies that working side group function contacts created the most hyper-functional muscle activity levels; far more than did balancing contacts.51,52
Interestingly, working side group function (a “prosthetic stabilization concept” applied to removeable prosthodontics) had long been believed to be “an effective way to distribute lateral occlusal forces on many teeth.”46–48 But this biomechanical concept of working side group function does not account for the fact that working side group function neuro-physiologically produces an excessive muscular response within fully dentate subjects.51,52 In all mock equilibration studies that promoted “Occlusion Plays no Role,” the authors failed to treat the main muscular hyperactivity agent by only performing CR-CO corrections and balancing side interference contact removal.7,40–45 The authors then reported no TMDs improvements because balancing interfering contacts do not generate sufficient muscle hyperactivity.51,52
Working side group function creates major muscular excitation because frequently from 6 to 10 opposing posterior working side teeth (Figure 4A) maintain multiple buccal and lingual transitory frictional excursive contacts, which simultaneously compress and flex many PDL and pulpal mechanoreceptors. This is what directly stimulates the Swallow Mechanism musculature into hyperfunction.20,52 But on the balancing side usually only 2 opposing teeth frictionally engage, and only on 2 to 4 opposing surfaces (Figure 4B). These few opposing contacts do not activate nearly as many periodontal ligaments or pulpal mechanoreceptors as the working side does. Multiple DTR treatment studies using the T-Scan 7-10/BioEMG III synchronization have shown that it is the high neural fiber volume activation of the working side that causes most TMDs muscular symptoms.25–37,52 That difference alone explains why the mock/real adjustment authors saw no marked TMDs symptom resolution.7,40–45
Further compounding this non-occlusal TMDs narrative was that the literature from that time (mid 1980s to mid 1990s) found only weak associations between static “Occlusal Factors” and TMDs symptoms. Factors like deep-bite, Class II orthodontic malocclusion, the CO-CR slide being coincident or not coincident, balancing contacts, and the maximum intercuspation of teeth,53 did not appear to be pathognomonic or significantly etiologic of TMDs. Many of these same “occlusal factors” were readily present in non-TMDs patients, whereby authors concluded that “occlusal factors” were not causative of TMDs.53 Further, an inciteful 1984 literature review that analyzed studies involving these “occlusal factors” determined that occlusal adjustment, as was subjectively performed in the mock/real equilibration studies7,40–45 was an unsatisfactory TMDs treatment, with poor improvement, and common relapse.54 This directed many educators away from pursuing an occlusal etiology, as the dental profession sought one universal treatment that would consistently and effectively manage all TMDs.
For this group of studies, their lack of functional occlusal force and timing data was their shortfall. They believed that they had adjusted the “correct teeth,” when in fact they had not adjusted the “correct teeth” at all. The main elements of these studies were that they included unmeasured and highly subjective occlusal adjustments. Four separate studies have shown that dentists using subjectivity (instead of measured data) select incorrect high force paper and ink markings 87-95% of the time.55–58 The mock equilibration study results have misled much of dentistry into believing their incorrect conclusions, instead of recognizing that their methods were flawed. From the early 1990s to the early 2000s, their findings were used to promote an alternative non-occlusal Somatic Symptom Disorder etiology for TMDs without obtaining scientific evidence to support it. The so-called “Biopsychosocial Etiology of TMDs” is a revisitation of the Myofascial Pain Dysfunction Syndrome. Importantly, naming MPDS “a syndrome” was and still is an admission that its’ etiology remains unknown. The term “Disorder” is also categorical admission of multiple conditions without a common etiology.
Over the past 3 + decades extensive occlusal adjustment research has been performed with the T-Scan 7-10/BioEMG III synchronized technologies and Disclusion Time Reduction (DTR) treatment. In all these studies the subjects’ occlusion had been objectively measured, and each study’s method has required researchers to obtain precise numerical time and force occlusal metrics to effectively perform the adjustments.57 DTR has routinely isolated and repeatedly eliminated the most common neuro-occlusal physiological etiology of muscular TMDs that is coincident with posterior Long Disclusion Time.11–19,22–37
Long Disclusion Time is sometimes present within each of the “occlusal factors” that prior authors thought might be contributory to TMDs (deep-bite, Class II, CO-CR slide, balancing contacts, and the maximum intercuspation of teeth).53,54 However, working side group function contacts are more often responsible for many long Disclusion Times. Clinicians and researchers who have not read the published DTR studies likely do not understand Disclusion Time Reduction’s significant contribution to occlusal neuroscience. Or perhaps they have misunderstood the TMDs treatment studies involving long Disclusion Time Reduction, which have consistently and dramatically reduced the symptoms of TMDs subjects.11–19,22–37
To understand how long Disclusion Time’s neuro-occlusion physiologically causes many muscular TMDs, one must first understand the occlusion’s unique neuroanatomy that promotes TMDs symptomatology.
SECTION III. The Unique Dental Occlusion Neuroanatomy and its Extensive Reach into and out of the Central Nervous System
The molar and premolar teeth are embryologically formed within the Parasympathetic Nervous System (PNS), which makes their pulp and Periodontal Ligament (PDL) mechanoreceptors peripheral nerves, able to sense the thickness of a red blood cell between occluding surfaces. Peripheral Nerves lie outside of the brain and spinal cord to generally make their initial synapse outside of the Central Nervous System (CNS) before entering the spinal column or the brain itself.59 However, despite being Peripheral Nerves, the molar and premolar pulp and Periodontal Ligament mechanoreceptors are the only afferent human peripheral nerves that enter the CNS directly via the Mesencephalic Nucleus, and without synapsing there, travel on further to the Trigeminal Motor Nucleus bilaterally to make their first synapse with efferent motor fibers to the muscles of mastication, the tensor tympani, the tensor veli palatini, the mylohyoid, and the anterior belly of the digastric muscles. This group of muscles facilitates the Swallow Mechanism.20 See Figures 5AB & 6AB. The same fibers also travel on to the Reticular Formation, which is the major brain waking center that controls alertness, circulation, respiration, swallowing, sleeping, and whole-body posture.20
Because of these unique neuroanatomic peripheral nerve pathways, opposing posterior tooth compressions that occur during chewing, clenching, bruxing, and swallowing, compress and flex the occluding molar and premolar pulp and PDL mechanoreceptor fibers. Masticatory muscle contractions are direct and without higher order modification, such that the patient cannot control or affect these contractions. See Figures 5AB & 6AB.
The Autonomic Nervous System (ANS)
The Parasympathetic Nervous System (PSNS) is one of the three divisions of the autonomic nervous system: the others being the sympathetic nervous system and the enteric nervous system.60,61 The enteric nervous system is sometimes considered part of the autonomic nervous system and sometimes considered an independent system.62 The autonomic nervous system regulates the body’s unconscious actions. The parasympathetic system is responsible for stimulating “rest-and-digest” or “breed and feed” activities that occur especially after eating and swallowing, including sexual arousal, salivation, lacrimation (tears), urination, digestion, and defecation.63 Its’ action is described as being complementary to the Sympathetic Nervous System (SNS), which is responsible for stimulating activities associated with the “fight-or-flight” response. See Figure 7.
Four preganglionic nerves (Oculomotor CN III, Facial CN VII, Glossopharyngeal CN IX and Vagus CN X) arise from specific nuclei in the Central Nervous System (CNS), which includes motor, sensory, sympathetic (CN III to the superior tarsal (eyelid) and dilator pupillae (dilation) muscles), and some parasympathetic fibers that all synapse at one of four parasympathetic ganglia:
-
Ciliary Ganglion within the orbit
-
Pterygopalatine
-
Otic
-
Submandibular
From these four ganglia, parasympathetic fibers from CN III, CN VII, and CN IX complete their journeys to their target tissues via the Cranial Nerve V’s trigeminal branches, using the ophthalmic (VI), maxillary (VII), and mandibular nerves (VIII).
The extensive neural reach of the occlusion into the Central Nervous System can be seen in Figure 7, which illustrates that fibers from the Trigeminal Nerve (CN V) are used by 3 other Cranial Nerves (CN III, VII, and IX) to reach their end structures. This means that because posterior tooth PDL and pulpal fibers reach the Reticular Formation (RetF) without a prior synapse, the posterior tooth motor nerve fibers communicate with the center of the brain, and five Cranial Nerves that are strongly associated with chewing, speaking, swallowing and breathing simultaneously (the Trigeminal CN V, the Oculomotor CN III, the Facial CN VII, Glossopharyngeal CN IX, and the Hypoglossal CN XII). And Cranial Nerves CN I and CN X also have minor associations with masticatory function.
The masticatory system is the most complex, most highly innervated, and most sensitive organ system in the body because the masticatory functions of chewing and speaking are far more complicated and precise than other functions outside of the brain.
The Neuro-Occlusal Physiology of Occlusion’s Direct Causative Role In TMDs
It has been consistently shown in T-Scan-based occlusal adjustment studies, that prolonged posterior excursive frictional contacts are etiologic for elevated muscular activity.11–19,22–37 In previous occlusal studies the authors thought they were diagnosing malocclusion from the interpretation of paper mark sizes, but due to the impossibility of successfully doing that they were treating without any diagnosis, which meant they were using pure guesswork.
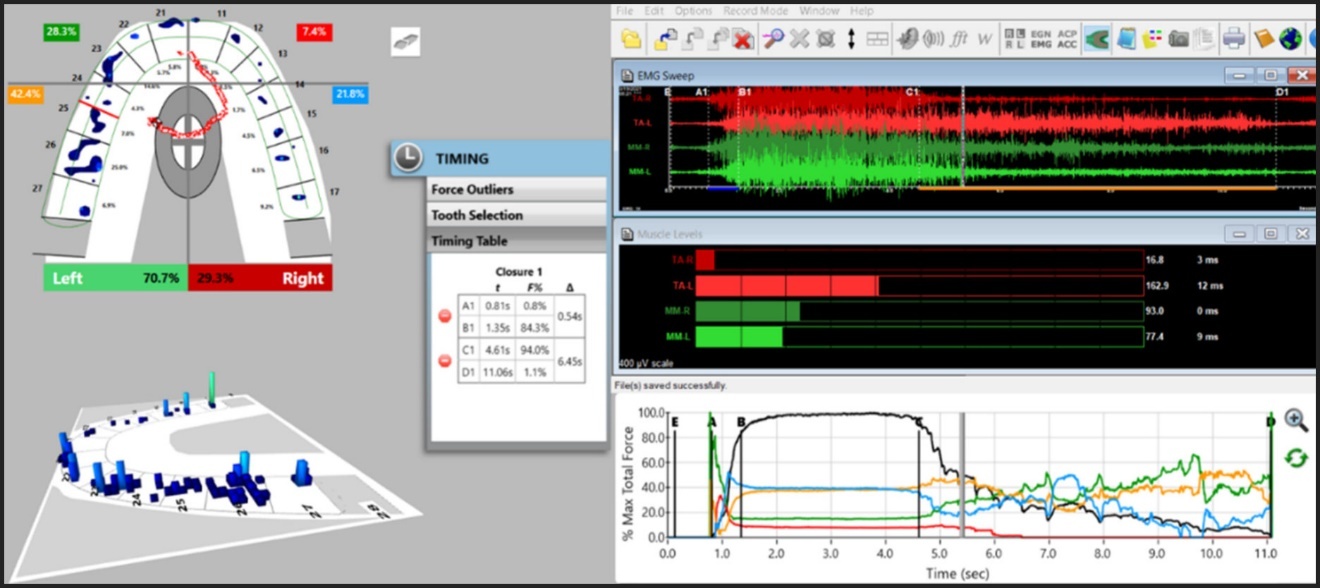
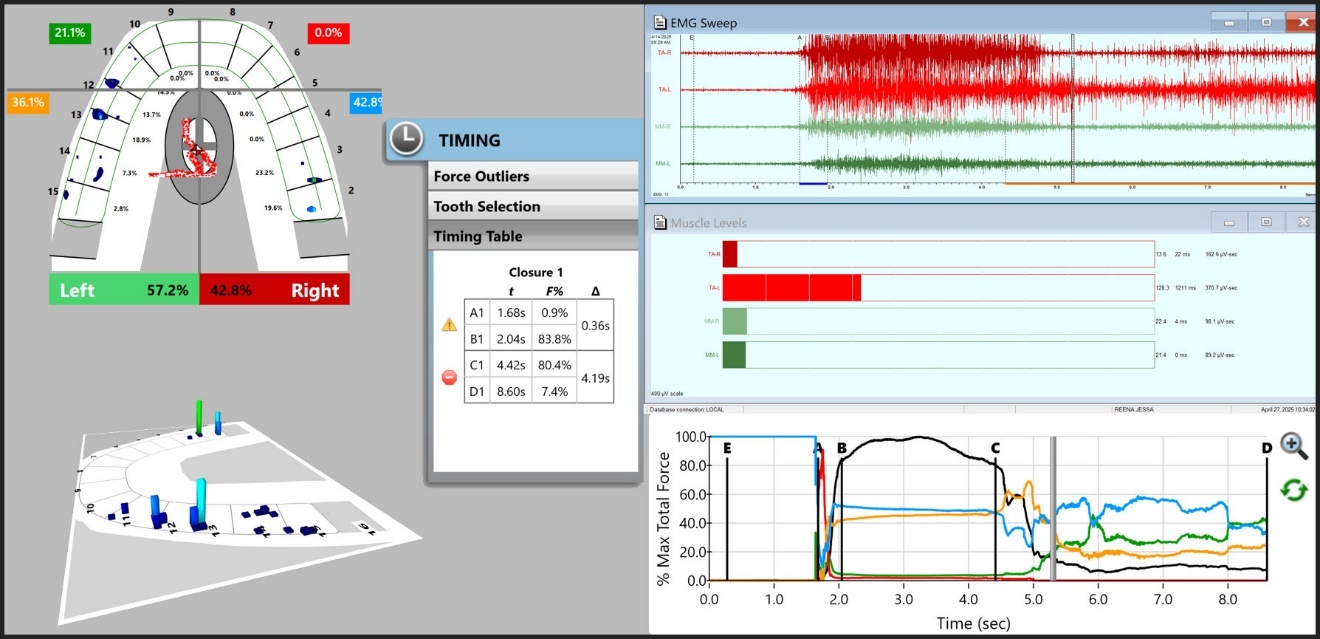
The mechanism of how muscular TMDs symptoms appear results from repeating pulpal flexure and PDL fiber compressions that occur during chewing food and swallowing, as well as during clenching and bruxing. Repeating pulpal flexures and PDL compressions that occur when posterior teeth frictionally engage during excursive movements increases muscle contractions beyond each muscle’s required baseline to perform routine daily functional and parafunctional movements. The elevated masticatory muscle contractions directly lead to muscular ischemia from ongoing lactic acid accumulation within these muscles (see Figure 8) that in susceptible patients, produces the clinical appearance of chronic painful TMDs symptoms.64 An example of this neuromuscular physiologic relationship between prolonged occlusal surface excursive friction and elevated masseter and temporalis muscle activity can be seen by recording excursive movements with the synchronized T-Scan 10/BioEMG III technologies (Figures 9 and 10).
Thus, TMDs muscular symptoms develop from the muscular ischemia induced by opposing tooth contacts that repeatedly engage during chewing, clenching, swallowing food, and breathing, that afferently elevate muscle contractions so that food is forced down into the esophagus without entering the lungs. Although parafunction is thought to be causative, most TMDs result from routine functional occlusal activities that hyperactivate the Swallow Mechanism musculature.20,64
SECTION IV. Two Methods that Alleviate TMDs Symptoms Using the Patients’ Own Physiology
As stated earlier, two long-term most successful TMDs treatments that clinicians utilize are:
-
The placement of a maxillo-mandibular orthotic, and/or
-
Disclusion Time Reduction (DTR) using the T-Scan 10/BioEMG III synchronized technologies.
An orthotic completely disengages the existing occlusion, while DTR has become the gold-standard method for the minimally invasive precise removal of only problematic functional occlusal interferences.11–19,22–37 These most successful treatment methods suggest that the common etiologies of TMDs are either:
-
Structural problems within the TMJ
-
A mal-posed maxillo-mandibular relationship (e.g., collapsed posterior bite)
-
The presence of occlusal interferences to function within the dentition.
All three structural aberrancies produce muscular pains from abnormal adaptive muscle activities, without any hint of myopathy or neuropathy, which may or may not coincide with muscle inflammation. Instead of trying to palliatively suppress the physiologically correct nociceptive pain signals going into the CNS, which report a dysfunction exists, correcting the structural and occlusal problems can permanently remove these neural signals, thereby permanently eliminating the TMDs symptoms. Of course, in multifactorial cases the reduction of symptoms may not be 100 %.
The many physical and emotional changes from treating the occlusion with Disclusion Time Reduction (DTR) therapy have been well documented since the first DTR study published in 1991.22 DTR therapy employs the Immediate Complete Anterior Guidance Development (ICAGD) coronoplasty first described in 1991,22 which reduces the occlusal surface excursive movement friction and significantly minimizes masticatory muscle hyperactivity.22,52,53 This is accomplished by reducing periodontal ligament and pulpal mechanoreceptor compression and flexure time-durations, which directly minimizes the output to the CNS from the unique peripheral neuroanatomy of the pulpal and PDL mechanoreceptor fibers.20
Figures 11 and 12 illustrate the rapid physiologic muscle activity reducing effects the ICAGD coronoplasty has on a TMDs patient’s left excursion. Another left excursion hyperfunctioning the left temporalis and masseter muscles can be seen in Figure 13. The post ICAGD reduced hyperactivity is shown in Figure 14.
The volume of existing DTR treatment research for muscular TMDs has significantly supported that the dental occlusion is a very common causative factor of many commonly seen TMDs in the head, face, ear, and neck, while the chronic pain involved drives the emotional symptoms associated with dysfunction.11–19,22–37
-
Chronic muscular TMDs symptoms have been predictably resolved many times
-
Functional chewing pattern improvements have been documented in DTR treated TMDs patients
-
Emotional depression resolution has been demonstrated in TMDs patients after undergoing DTR
-
Headaches and migraines have been resolved in TMDs patients after undergoing DTR
-
Temporomandibular Joint structural pathology improvements have been documented in DTR treated TMDs patients
-
Multi-Center Randomized Controlled Disclusion Time Reduction (DTR) Trials (RCT) resolved chronic TMDs symptoms in the treated TMDs patients
-
Bruxism frequency reductions and pain level reductions have been documented in TMDs patients after DTR
-
Peri-Implant bone preservation around posterior implant prostheses that occluded against natural teeth have been documented in implant patients after DTR
-
Cold Dentinal Hypersensitivity (CDH) improvements have been documented in TMDs patients after DTR
-
Meniere’s Disease (MD) hearing improvements have been documented in TMDs patients after DTR
-
Trigeminal Neuralgia (TN) pain reductions have been documented in TMDs patients after DTR
-
Whole body postural alignment improvements have been documented in TMDs patients after DTR
Many clinicians and international researchers have successfully adopted the principles of DTR in diagnosis and during definitive treatment planning with orthotics, coronoplasty, comprehensive restoration and orthodontics. Clinicians and researchers who do not use digital occlusal analysis with the T-Scan 7-10/BioEMG III for diagnosing or treating the occlusion predictably, rely on indefinite term palliative care that has a much lower TMDs resolution success rate. For many years now, prominent dental journal editors have resisted publishing T-Scan based research, while some lecturers have disavowed the T-Scan technology’s sensor components. Further, some systematic review authors have exhibited anti-technology biases and have excluded relevant T-Scan 7-10/BioEMG III and DTR treatment studies from their reviews. These exclusions prevented some in dentistry from learning how effective DTR therapy has been in solving TMDs, which has resulted in fewer chronic pain patients receiving the effective TMDs care that DTR provides.
SECTION V. The Consistent Failures of Pharmacological and Psychosocial Treatments of TMDs
Medication trials as well have not been proven effective in resolving painful TMDs. In one Meprobamate study (a schedule IV barbiturate),65 the authors claimed that 52 of 90 patients taking the drug reported “some improvement,” while half as many (28) reported improvement after taking a placebo. In a more recent double-blind, randomized controlled clinical trial comparing a placebo to both diazepam and ibuprofen, Singer et al., found only diazepam significantly reduced pain.8 The authors concluded “the lack of effect following administration of an anti-inflammatory analgesic [NSAID] suggests that inflammation is not the basis for chronic muscle pain in the orofacial region, and that the analgesic effect of such medications does not offer sufficient pain relief in this (TMDs) condition.”8
To date, despite the long-term promotion of psychological treatment as a valid chronic TMDs treatment, the few attempted Cognitive Behavioral Therapy (CBT) treatment studies, done in combination with “usual treatments,” (meaning flat-plane splints), have poorly resolved painful TMDs physical symptoms.10
MPDS theory has not survived scientific scrutiny
Laskin et al., also tested a placebo drug and claimed that 26 of 50 TMDs patients reported some improvement in their condition.2 The authors went on to state, “these findings indicate that psychological factors that are inherent in the conventional doctor-patient relationship should be recognized, because they can be used advantageously for the treatment of patients with MPD syndrome.”2 This suggestion insinuated that exploiting a patient’s emotions might aid in resolving physical pains. Unfortunately, no study has successfully demonstrated that in-vivo since 1972.
In a further attempt to validate their MPDS theory, the same authors also claimed that 28 of 71 MPDS patients (39%) showed remission or noticeable improvement in their symptoms with the use of a non-occluding appliance that did not directly modify any occlusal contacts or alter mandibular positioning."7 However, this unsupported claim has not been made since and there is more recent literature explaining that a non-occlusal splint cannot be a true placebo, since it does alter tongue and/or jaw position.66,67
Greene and Laskin also performed three placebo studies that recruited 120 MPDS patients,4,6,41 reporting that “certain types of patients tended to respond favorably to placebos, while others did not,” implying that symptomology is strongly dependent on personality type. However, the fact that no one has been able to duplicate their results since 1979 calls into question their methods. During a site visit by a committee from the NIDCR who were considering a grant extension in the early 1980s, a graduate student admitted to being told by the study investigators “to make sure the patient surveys were answered in support of our theory.”41 After this unscientific approach was discovered, funding for additional MPDS research was denied. Since that time, no other study has been published that duplicated Greene and Laskin’s placebo TMDs patient responses. Further, more recent Randomized Controlled Trials definitively determined that occlusal splints were significantly more effective than placebo splints.68,69
Dismissing Occlusion as an Etiology for TMDs has been Contrived
The only self-rationalization one can use to thoroughly dismiss occlusion as a causative etiology for TMDs is to cling to the belief that TMDs are Somatic Symptom Disorders (SSD), previously referred to as a “psychosomatic mental illness.”4,7
That claim of an SSD etiology for TMDs requires one to actively believe that:
-
TMDs signs are coincidental without being etiologic
-
TMDs symptoms are mostly hysterical
-
Oral appliances and computer-guided occlusal adjustments resulting in long-term TMDs pain relief, providing measurable improvements in masticatory function, and controlling TMDs symptoms are just “miraculously effective placebos.”
It has also been popular to use psychometric instruments like the Beck Depression Inventory II, the SCL-90 and the PHQ-15 to document that many TMDs patients often exhibit depression, anxiety, and/or may falsely appear to have a Somatic Symptom Disorder (SSD). It is highly denigrating to the TMDs patient population who live with chronic painful physical symptoms to be labeled “psychosomatic”, when their physical pains can often be successfully resolved.11,14,33 Emotional disturbances in TMDs patients are well documented, but often the authors who used psychometric tests with TMDs patients failed to go back after occlusal treatment was rendered and re-apply those same psychometric measurements. Alternatively, the Beck Depression Inventory (BDI-II) was used in T-Scan 10/EMG DTR studies before and after treated subjects had their long Disclusion Times shortened, whereby rapid and lasting psychometric emotional improvements were obtained in moderate to severely depressed chronic TMDs patients.11,14,33
Consider that the lead author of the Research Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD) subsequently made this claim regarding SSDs, “True somatization disorder is very rare (< 1%) and requires a DSM-III-R diagnosis of at least 13 different physical symptoms which cannot be explained by, or are in gross excess of physical findings, and have caused the patients to seek health care or alter their lifestyles.”70 How many dentists are properly qualified to establish this diagnosis?
CONCLUSIONS
The idea that “Occlusion has no role in TMDs” was borne out of occlusal adjustment studies that didn’t treat the true causative agent of occlusally-driven TMDs physical symptoms and pain. The belief that Working Side Group Function contacts were “distributing forces across many teeth” led mock equilibration and real equilibration study authors to not treat the working side. By only treating CR-CO and balancing side contacts, both mock and real adjustment patients responded middling to poor in many occlusal adjustment studies performed prior to the T-Scan I’s evolution and the discovery of Long Disclusion Time.
The fact that TMDs patients are often emotionally affected by the severe pain associated with TMDs comes as no surprise. However, the claim that the emotional factors are etiological of TMDs remains unsupported by any scientific literature. In contrast to SSD etiology, occlusion has repeatedly been shown to be a correctible physical cause of TMDs, supported in the dental literature with many repeated studies that demonstrated the definitive effectiveness of occlusal treatments. When the patient’s TMJs are functionally intact, Disclusion Time Reduction (DTR) occlusal treatment has been consistently highly effective since it was discovered in 1991. When TMDs patients have TMJs that are structurally compromised, occlusal appliances have been the treatment of choice for over 5 decades.
Funding Statement
No funds or in-kind offers were received from any source for the production of this review.
Disclosures
Robert B. Kerstein is a former Assistant Clinical Professor at Tufts University School of Dental Medicine. Boston USA. He has no financial arrangements with any dental manufacturer and receives no compensation from sales of any dental product. Ben A. Sutter operates a private practice in Eugene, OR USA, is an Adjunct Professor UNLV School of Dental Medicine Department of Clinical Sciences and faculty at VIVOS Institute in Denver, CO USA. He has no financial arrangement with any dental manufacturer and receives no compensation from sales of any dental product. John Radke is the Chairman of the Board of Directors of BioResearch Associates, Inc., Milwaukee, WI, USA. He receives no commission from the sales of any products.
Communicating author
Robert B. Kerstein - tmjdoc@ix.netcom.com



_from_molar_and_premolar_pulp_and_pdl_.jpeg)
._**b.**.jpeg)


_when_synchronized_with_the_.jpg)

)_mid_left_excursion_after_icagd_was_rendered_.jpeg)





_from_molar_and_premolar_pulp_and_pdl_.jpeg)
._**b.**.jpeg)


_when_synchronized_with_the_.jpg)
)_mid_left_excursion_after_icagd_was_rendered_.jpeg)